- LOGIN
- MemberShip
- 2025-12-22 09:28:24
- ‘Adempas, effective alternative for patients with inadequate response to PDE5i’
- by Son, Hyung Min | translator | 2025-12-22 08:53:59
‘The ultimate goal for PAH is to reach and maintain a low-risk status. If this goal is not achieved or the risk level is not sufficiently lowered, an early change in treatment strategy is essential.”
Switching to Bayer’s sGC stimulator ‘Adempas (riociguat)’ is emerging as a practical treatment strategy for patients with PAH who do not show sufficient response to PDE5 inhibitors. With the recent establishment of reimbursement criteria in Korea, experts note that a turning point has been created in a treatment landscape that has long relied on sequential monotherapy.
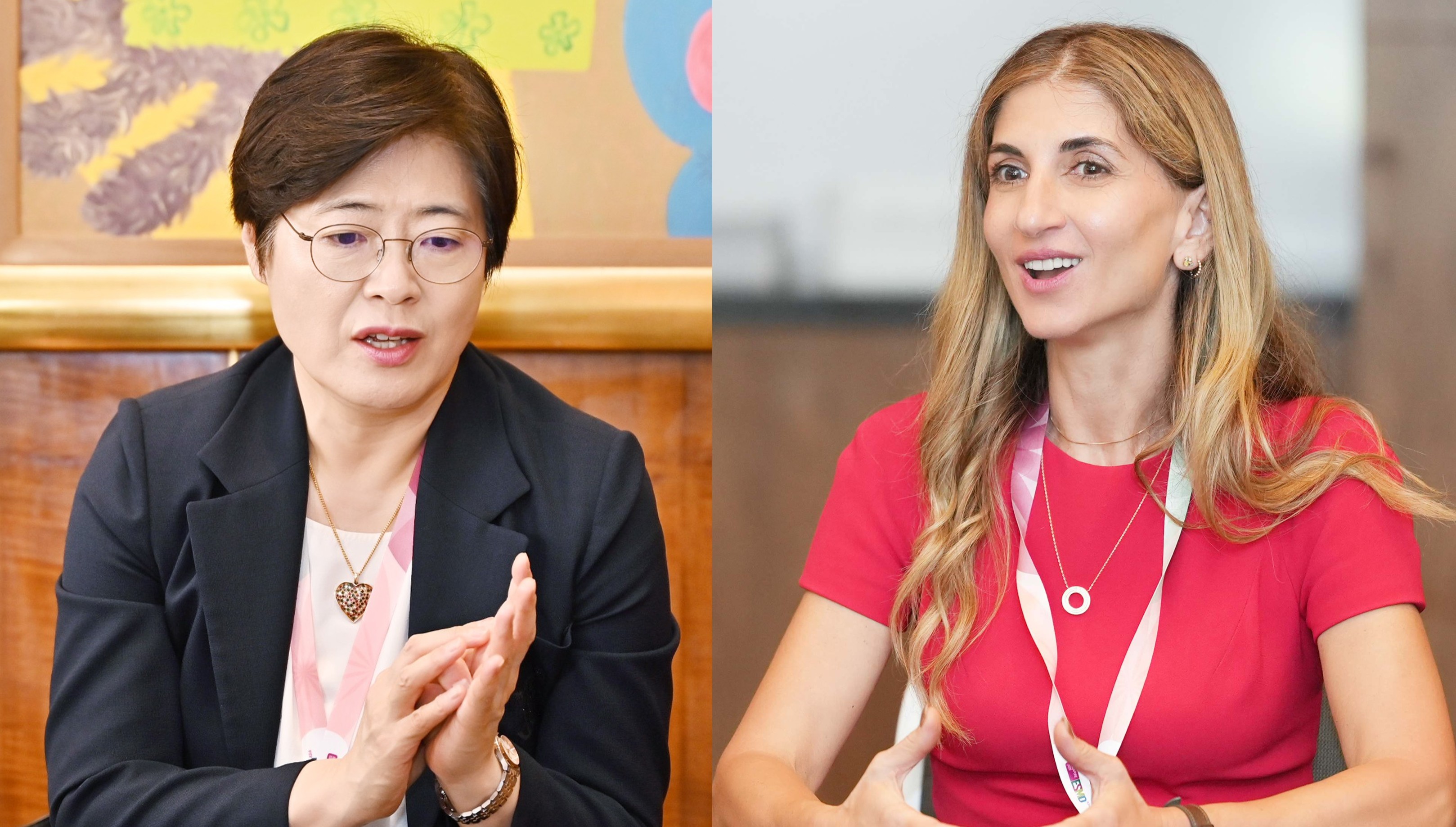
Vallerie McLaughlin, Professor of Cardiovascular Medicine at the University of Michigan Medical Center, and Wook-Jin Chung, Professor of Cardiology at Gachon University Gil Medical Center, recently emphasized the clinical potential of Adempas in PAH treatment during a recent interview with Daily Pharm.

Pulmonary hypertension, characterized by abnormally elevated pulmonary arterial pressure, is classified into five groups based on etiology. Among these, Group 1 PAH and Group 4 chronic thromboembolic pulmonary hypertension (CTEPH) are considered rare diseases, accounting for only about 3% of all pulmonary hypertension patients each. Often beginning with nonspecific symptoms like shortness of breath, fatigue, and dizziness, patients frequently attribute these to aging or are misdiagnosed with other conditions at primary care facilities, leading to significant diagnostic delays.
PAH is known to be a severe, life-threatening condition, with a mortality risk within 2-3 years if left untreated. In Korea, the number of diagnosed patients has increased due to greater physician awareness, efforts toward early detection, and wider use of right heart catheterization. However, concerns remain that the domestic treatment environment still diverges in part from global clinical guidelines.
Unlike international guidelines that recommend initial combination therapy with endothelin receptor antagonists (ERA) and phosphodiesterase type 5 inhibitors (PDE5i) from the outset, sequential monotherapy-based treatment strategies remain commonly applied in Korea.
PAH treatments are categorized by mechanism of action into: ▲ Endothelin receptor antagonists (ERAs) ▲ Nitric oxide pathway targeted therapies (PDE5 inhibitors, sGC stimulators) ▲ Prostacyclin analogues (PCAs) ▲ Prostaglandin receptor agonists (PRAs). Global guidelines recommend initiating treatment with a combination of ERA and PDE5 inhibitors from the outset, escalating treatment by adding agents with different mechanisms, such as PCA or PRA, when treatment response is inadequate. This strategy aims to maximize therapeutic efficacy by simultaneously targeting multiple pathophysiological pathways.
In contrast, the domestic approach has primarily involved initiating treatment with ERA monotherapy, adding a PDE5 inhibitor if response is inadequate, and subsequently combining PCA or PRA if improvement is still lacking. However, studies report that despite the use of a combination of ERA and PDE5 inhibitors, some patients experience clinical deterioration due to inadequate response to PDE5 inhibitors or issues related to tolerability.
In this context, Adempas (riociguat), an sGC stimulator, is gaining attention as a potential treatment option to replace PDE5 inhibitors.
In the REPLACE study, which enrolled adult patients with symptomatic pulmonary arterial hypertension (PAH) who showed an inadequate clinical response to PDE5 inhibitor therapy, patients who switched from a PDE5 inhibitor to Adempas achieved a 2.78-fold higher rate of clinical improvement at 24 weeks compared with those who continued PDE5 inhibitor treatment. and a 90% reduction in the risk of clinical worsening.
Based on this evidence, the 2022 ESC/ERS (European Society of Cardiology/European Respiratory Society) pulmonary hypertension treatment guidelines also recommend switching from PDE5 inhibitors to sGC stimulators in patients who fail to reach treatment goals despite ERA and PDE5 inhibitor combination therapy.
Accordingly, reimbursement criteria for Adempas were newly established in Korea starting this June. Reimbursement is now granted for patients with PAH (WHO Group 1) in WHO functional class II-III who either ▲show insufficient response to ERA and/or PDE5 inhibitor therapy or ▲have contraindications to both ERA and PDE5 inhibitors. This is expected to serve as a new treatment strategy that can improve patient status before escalating to triple combination therapy.
Amid these changes, the two professors emphasized, “Suspicion is the starting point in pulmonary hypertension. Alongside the importance of early diagnosis, treatment goals should be set to reach and maintain the low-risk status, with treatment strategies flexibly adjusted based on patient response.”
Q. Please explain the main symptoms and causes of pulmonary arterial hypertension, along with its severity.
Professor Vallerie McLaughlin: PAH is characterized by prominent shortness of breath during exercise or activity. While the timing varies among patients, they commonly experience dyspnea. In fact, many patients seek medical care primarily due to this shortness of breath. Other symptoms include fatigue, dizziness, chest pain, and leg swelling. These symptoms are non-specific and can commonly occur in other diseases, often leading to delayed diagnosis.
PAH is a rare disease. While some cases are idiopathic with no identifiable cause, they can also result from genetic factors, specific medications, dietary habits, or conditions like connective tissue disorders, liver disease, or heart failure.
Professor Wook-Jin Chung: The hallmark symptom of PAH is shortness of breath when climbing stairs or hills. Patients may not feel breathless on flat ground, but even mild exertion, such as ascending stairs, can provoke significant dyspnea. Diagnosis is often delayed because symptoms such as fatigue, dizziness, and chest pain are nonspecific.
Although advances in drug development have made PAH a more manageable condition, prognosis remains poor. Therefore, prompt evaluation by specialized clinicians, accurate diagnosis, and appropriate treatment are critically important.
Q. How do the treatment environments for pulmonary arterial hypertension differ between the United States and Korea?

Professor Vallerie McLaughlin: In the United States, 13 PAH drugs have already received FDA approval and are available for use. In practice, many patients are using a diverse class of medications, including endothelin pathway–targeting agents (ERA), prostacyclin pathway–targeting agents (PCA, PRA), and nitric oxide pathway–targeting agents (PDE5 inhibitors and sGC stimulators).
Patients classified as high risk require more intensive treatment. For these patients, triple combination therapy may be considered, including intravenous prostacyclin pathway agents in combination with endothelin or nitric oxide pathway therapies.
Patients in the intermediate-risk or low-risk groups receive dual therapy based on oral medications, using agents such as ERAs or nitric oxide pathway therapies, including PDE5 inhibitors or sGC stimulators.
Initial treatment, however, is only the first step. After 3-4 months of treatment initiation, the patient's risk level must be periodically reassessed using objective evaluation tools. If treatment goals have been achieved, the current regimen can be maintained. However, if the risk level remains insufficiently reduced, treatment intensity must be escalated. Strategies such as triple combination therapy or switching from the previously used PDE-5 inhibitor to an sGC stimulator can be considered. This re-evaluation process is repeated thereafter, with the ultimate treatment goal of achieving and sustaining a low-risk status for the patient.
Professor Wook-Jin Chung: Globally, the development of PAH therapies gained momentum with the launch of epoprostenol in 1995. In Korea, effective treatment became possible in 2005, when Bayer’s Ventavis (iloprost) was approved for reimbursement.
In the past, treatment escalation was typically initiated only after clinical deterioration. However, because PAH is difficult to cure, waiting for disease progression before intensifying treatment is highly risky and insufficient to reduce mortality. Consequently, recent treatment strategies follow the principle of guideline-directed medical therapy (GDMT), which emphasizes a goal-oriented approach—lowering risk early, achieving a low-risk state, and maintaining it over time.
In addition to guiding patients toward a low-risk status, another important treatment goal is to normalize hemodynamic parameters as much as possible.
The minimum goal is to sustain a low-risk state by maintaining a mean pulmonary artery pressure (mPAP) ≤40 mmHg and pulmonary vascular resistance (PVR) ≤4 Wood units. Some patients achieve near-normal levels, such as a mPAP ≤20 mmHg and PVR ≤2 Wood units.
Injection therapy is required in only about 10% of all patients, and the majority of patients can achieve hemodynamic goals with oral therapies alone.
Q. Please share any treatment challenges you have encountered in clinical practice.

Professor Wook-Jin Chung: One of the main challenges in treatment is that several therapies used globally have not yet been introduced in Korea. While 13 types of medications are used globally, 4 of them have not been introduced in Korea. Even among the approved drugs, some are not covered by reimbursement, limiting patient access.
According to the National Cancer Information Center, Korea's overall five-year cancer survival rate (2018-2022) is approximately 72.9%, whereas the five-year survival rate for PAH is 71.9%. Given that PAH has a poorer prognosis than cancer, government support is essential.
Only a portion of PAH patients qualify for a special calculation exception, and even then, this is limited to idiopathic pulmonary arterial hypertension (IPAH). PAH is a high-cost disease where treatment is virtually impossible without insurance support. Therefore, beyond IPAH, it is necessary to expand special reimbursement programs to include PAH caused by other etiologies, based on accurate disease classification.
In Korea, PAH treatment typically begins with ERA, with PDE-5 inhibitors added if the response is insufficient. However, there was no subsequent alternative for patients who did not respond adequately to PDE-5 inhibitors. Since intravenous formulations were not introduced domestically, subcutaneous injection and inhalation formulations of prostacyclin pathway-targeted therapies were used.
With the recent inclusion of Adempas under reimbursement, a new option has emerged. As an sGC stimulator, Adempas produces a strong vasodilatory effect even at low doses, making it a powerful option for patients who do not respond adequately to PDE-5 inhibitors. It can be used immediately as a switch option in patients with poor PDE-5 inhibitor response and is also available in cases where PDE-5 inhibitors are contraindicated. Clinically, this represents a highly meaningful and practical addition to the treatment landscape.
Q. Adempas has been used clinically in the US for a long time. How would you assess its clinical value?
Professor Vallerie McLaughlin: Adempas has been used as a treatment for PAH in the US for over a decade, accumulating substantial clinical data over this extended period.
Adempas is a drug that directly promotes cGMP production, independent of nitric oxide (NO) levels in the body. Unlike PDE-5 inhibitors, it induces vasodilation and achieves therapeutic effects for PAH in an NO-independent manner, even without the precursor substance NO.
In the PATENT clinical trial, which confirmed the therapeutic efficacy and safety of Adempas compared to placebo, significant improvements were observed in exercise capacity (including the 6-minute walk test), pulmonary vascular resistance, and cardiovascular markers, including NT-proBNP, compared to placebo.
In addition, the REPLACE study compared treatment outcomes by dividing patients previously receiving combined ERA and PDE-5 inhibitor therapy into two groups: one maintaining existing therapy and the other switching the PDE-5 inhibitor to Adempas. Results showed the clinical improvement rate upon switching to Adempas was 2.78 times significantly higher than in the group that continued PDE-5 inhibitor therapy.
Given Korea’s limited access to PAH therapies, switching to Adempas represents an effective alternative for patients who show an inadequate response to PDE-5 inhibitors.
Q. What is the value of using Adempas for the treatment of CTEPH?
Professor Wook-Jin Chung: Adempas is the only medication available for patients with chronic thromboembolic pulmonary hypertension (CTEPH) and has been used worldwide for over a decade. However, in Korea, it is not covered by insurance, resulting in low patient access.
The estimated number of CTEPH patients is nearly comparable to that of pulmonary arterial hypertension patients, but only about 300 to 400 patients actually receive treatment, such as surgery or interventions. Adempas is beneficial for CTEPH patients who still have residual pulmonary artery pressure after intervention or for those who are ineligible for surgery or procedures.
Given its strong clinical evidence, it is essential to establish a KCD code for CTEPH and ensure access to the drug through reimbursement coverage. Academic societies plan to continue discussions with the National Assembly and HIRA on this issue.
Professor Vallerie McLaughlin: Adempas is the only FDA-approved treatment for CTEPH and has been used in real-world clinical practice in the United States for over a decade.
It is indicated for patients with CTEPH whose occluded vessels are too small for surgical or interventional procedures like pulmonary endarterectomy or balloon angioplasty, or for whom pulmonary artery pressure remains elevated after such procedures.
Even among patients who undergo pulmonary endarterectomy, pulmonary artery pressure sometimes remains persistently high after surgery. Because persistently high pressure negatively impacts prognosis, pulmonary artery pressure is reassessed at 6 months post-surgery via right heart catheterization. According to UK research, patients whose mean pulmonary artery pressure does not decrease below 35 mmHg post-surgery are known to have a very poor prognosis. For these patients, measures to lower pulmonary artery pressure using Adempas are implemented.
There is also evidence that pre-treatment with Adempas before balloon pulmonary angioplasty can reduce surgical risk. Based on these data, Adempas is actively used across various CTEPH patient populations, with successful clinical outcomes.
Q. What treatment options are used for CTEPH patients who are not eligible for surgery or intervention?
Professor Wook-Jin Chung: Some patients are currently using PDE-5 inhibitors without reimbursement, which reflects the treatment gap caused by the unavailability of Adempas. This highlights the urgent need to establish a KCD code and reimbursement coverage for CTEPH.
Professor Vallerie McLaughlin: ERA-class drugs were studied in CTEPH patients in the past, but the results were not successful. Adempas is the only therapy that has demonstrated significant efficacy in CTEPH, and because there are no viable alternatives, the need for its access is even more pressing.
Q. What recommendations would you make to improve the pulmonary hypertension treatment environment?
Professor Vallerie McLaughlin: Raising awareness of the disease is paramount. Because pulmonary hypertension presents with highly nonspecific symptoms, diagnosis is often delayed. The media also plays a crucial role in this process. Providing the public with clear information about symptoms that should raise suspicion of pulmonary hypertension can greatly facilitate early diagnosis and treatment.
Given that experts have already established a robust clinical network, specialized institutions should take on a central role as pulmonary hypertension referral centers. This would enable efficient referral systems, allowing suspected cases identified in primary care settings to be promptly transferred to specialized centers. Clinicians should perform appropriate risk assessments each time a patient visits the hospital and, when necessary, stepwise intensify treatment to reduce risk and lower long-term mortality.
Professor Wook-Jin Chung: In Korea, expanding access to medications is the first priority. Introducing new drugs and using them appropriately according to guidelines is crucial for improving treatment outcomes.
Furthermore, designating and operating specialized pulmonary hypertension centers is essential. The designation of these so-called ‘Centers of Excellence’ significantly impacts treatment outcomes. Therefore, government-level support is absolutely necessary. I would like to emphasize that a specialized pulmonary hypertension center covering all five types of pulmonary hypertension, not just PAH, needs to be established.
We plan to continue the “Lung, Early” awareness campaign to improve understanding of pulmonary hypertension among the public, healthcare professionals, and policymakers, and to maintain discussions with pharmaceutical companies and the government to facilitate access to new therapies. We are also collecting data and conducting research to build a patient-centered treatment environment in Korea, with ongoing efforts to improve care across the entire spectrum of pulmonary hypertension, including PAH.
Some patients use PDE-5 inhibitors without reimbursement, but this represents the treatment gap arising from the inability to use Adempas. This underscores the urgency of establishing a new KCD code for CTEPH and securing insurance coverage.
-

- 0
댓글 운영방식은
댓글은 실명게재와 익명게재 방식이 있으며, 실명은 이름과 아이디가 노출됩니다. 익명은 필명으로 등록 가능하며, 대댓글은 익명으로 등록 가능합니다.
댓글 노출방식은
댓글 명예자문위원(팜-코니언-필기모양 아이콘)으로 위촉된 데일리팜 회원의 댓글은 ‘게시판형 보기’와 ’펼쳐보기형’ 리스트에서 항상 최상단에 노출됩니다. 새로운 댓글을 올리는 일반회원은 ‘게시판형’과 ‘펼쳐보기형’ 모두 팜코니언 회원이 쓴 댓글의 하단에 실시간 노출됩니다.
댓글의 삭제 기준은
다음의 경우 사전 통보없이 삭제하고 아이디 이용정지 또는 영구 가입제한이 될 수도 있습니다.
-
저작권·인격권 등 타인의 권리를 침해하는 경우
상용 프로그램의 등록과 게재, 배포를 안내하는 게시물
타인 또는 제3자의 저작권 및 기타 권리를 침해한 내용을 담은 게시물
-
근거 없는 비방·명예를 훼손하는 게시물
특정 이용자 및 개인에 대한 인신 공격적인 내용의 글 및 직접적인 욕설이 사용된 경우
특정 지역 및 종교간의 감정대립을 조장하는 내용
사실 확인이 안된 소문을 유포 시키는 경우
욕설과 비어, 속어를 담은 내용
정당법 및 공직선거법, 관계 법령에 저촉되는 경우(선관위 요청 시 즉시 삭제)
특정 지역이나 단체를 비하하는 경우
특정인의 명예를 훼손하여 해당인이 삭제를 요청하는 경우
특정인의 개인정보(주민등록번호, 전화, 상세주소 등)를 무단으로 게시하는 경우
타인의 ID 혹은 닉네임을 도용하는 경우
-
게시판 특성상 제한되는 내용
서비스 주제와 맞지 않는 내용의 글을 게재한 경우
동일 내용의 연속 게재 및 여러 기사에 중복 게재한 경우
부분적으로 변경하여 반복 게재하는 경우도 포함
제목과 관련 없는 내용의 게시물, 제목과 본문이 무관한 경우
돈벌기 및 직·간접 상업적 목적의 내용이 포함된 게시물
게시물 읽기 유도 등을 위해 내용과 무관한 제목을 사용한 경우
-
수사기관 등의 공식적인 요청이 있는 경우
-
기타사항
각 서비스의 필요성에 따라 미리 공지한 경우
기타 법률에 저촉되는 정보 게재를 목적으로 할 경우
기타 원만한 운영을 위해 운영자가 필요하다고 판단되는 내용
-
사실 관계 확인 후 삭제
저작권자로부터 허락받지 않은 내용을 무단 게재, 복제, 배포하는 경우
타인의 초상권을 침해하거나 개인정보를 유출하는 경우
당사에 제공한 이용자의 정보가 허위인 경우 (타인의 ID, 비밀번호 도용 등)
※이상의 내용중 일부 사항에 적용될 경우 이용약관 및 관련 법률에 의해 제재를 받으실 수도 있으며, 민·형사상 처벌을 받을 수도 있습니다.
※위에 명시되지 않은 내용이더라도 불법적인 내용으로 판단되거나 데일리팜 서비스에 바람직하지 않다고 판단되는 경우는 선 조치 이후 본 관리 기준을 수정 공시하겠습니다.
※기타 문의 사항은 데일리팜 운영자에게 연락주십시오. 메일 주소는 dailypharm@dailypharm.com입니다.