- LOGIN
- MemberShip
- 2025-12-17 06:01:01
- ADCs in the frontline in triple-negative breast cancer
- by Son, Hyung Min | translator | 2025-12-12 07:54:16
“In the metastatic stage, nearly half of breast cancer patients still do not survive beyond five years. A significant number of HER2-overexpressing patients experience disease progression within two years after first-line treatment, and those with triple-negative breast cancer (TNBC) relapse even faster due to the lack of targeted treatment options. Ultimately, providing stronger therapeutic options earlier in the treatment sequence is key to improving survival.”
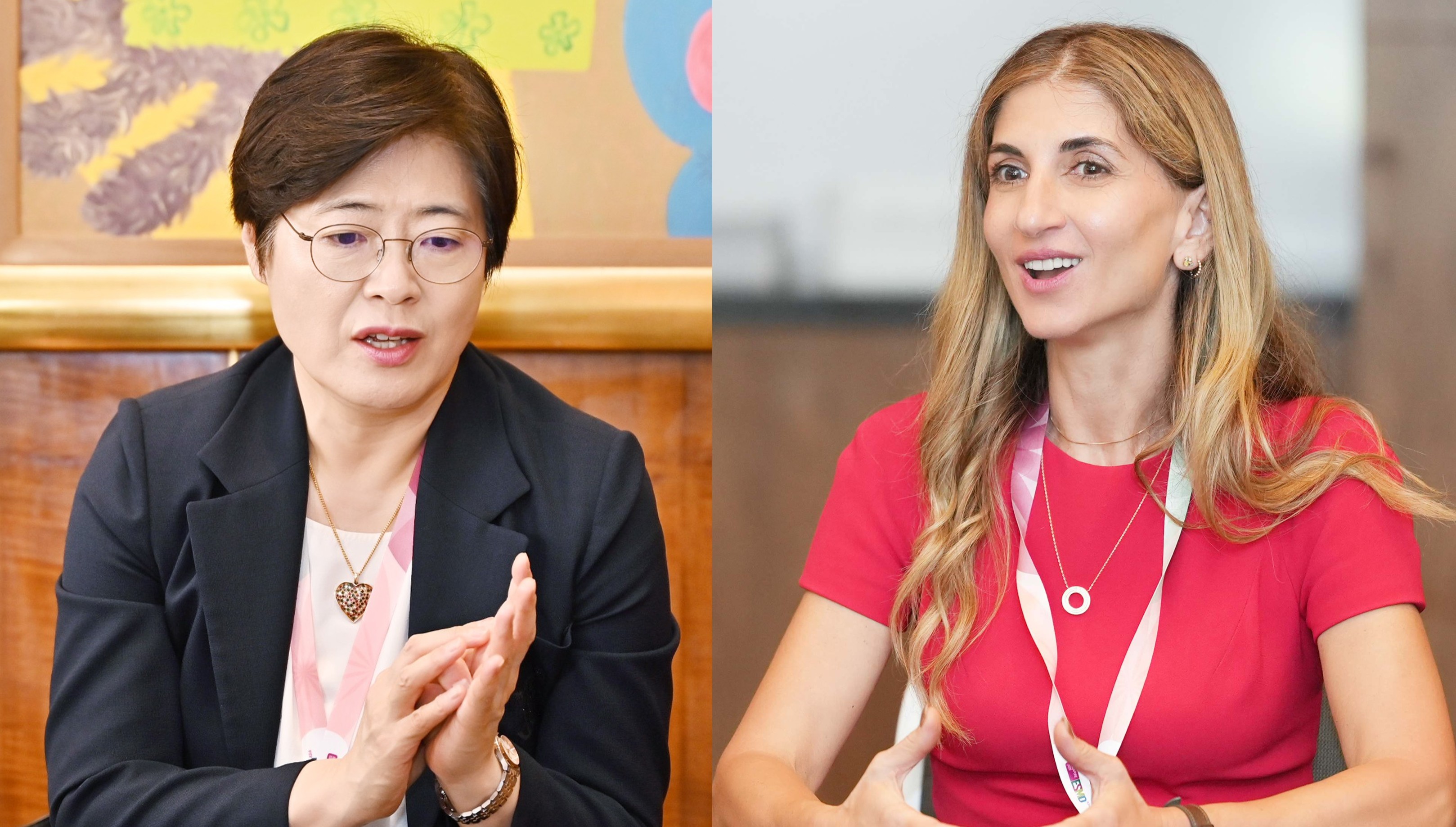
Professors Sung-Bae Kim (Medical Oncology, Asan Medical Center) and Kyong-Hwa Park (Medical Oncology, Korea University Anam Hospital) stressed the above during an interview with journalists at ESMO Asia 2025 in Singapore, noting that the greatest unmet need in metastatic breast cancer is redefining effective first-line treatment strategies.

For metastatic breast cancer, the realistic goal remains not a cure, but how long and how well patients can endure. This is because while the 5-year survival rate for early-stage breast cancer exceeds 99%, the 5-year survival rate for patients diagnosed at the metastatic stage is only about 49%. In particular, the subtype and treatment strategies for metastatic breast cancer are completely divided based on HER2 and hormone receptor (HR) expression, with distinct unmet needs remaining for each subtype.
For HER2-positive breast cancer with HER2 overexpression, survival extension has been achieved over the past decade with the so-called ‘THP regimen’ (taxane + Herceptin (trastuzumab) + Perjeta (pertuzumab)). However, in reality, disease progression occurs within two years in a significant number of patients, and brain metastases develop in about 25%, highlighting its limitations.
The most aggressive subtype, triple-negative breast cancer (TNBC), which lacks expression of HER2, HR, and estrogen receptors, has a high rate of distant metastasis within 5 years of diagnosis and a sharply elevated risk of recurrence between 1-2 years post-diagnosis. However, the limited availability of targetable therapies remains a significant challenge.
As a result, the importance of frontline therapy is becoming increasingly important in the field. In metastatic breast cancer, drug treatments tend to show a clear decline in efficacy as treatment lines progress. This means that the effectiveness of therapies deployed in the earlier treatment sequence, when patients are in relatively good condition, can significantly influence the overall survival curve.
In the DESTINY-Breast09 trial, the HER2-targeted antibody-drug conjugate (ADC) ‘Enhertu (trastuzumab deruxtecan)’ extended progression-free survival (PFS) by approximately 1.5 times (40.7 months) compared to the THP regimen, which has been the first-line standard for HER2-positive metastatic breast cancer for over a decade, signaling a paradigm shift in first-line treatment. Particularly noteworthy is its consistent benefit even in high-risk subgroups, such as those with brain metastases or PIK3CA mutations.
Signs of change also emerged in TNBC. Until now, only a subset of PD-L1-positive TNBC patients could receive immunotherapy, while the remaining 60-70% of patients had to rely on cytotoxic anticancer drugs, which are highly toxic and frequently develop resistance. The Trop-2-targeted ADC ‘Datroway (datopotamab deruxtecan)’ emerged as a key first-line ADC-based option in this field. In the Phase III TROPION-Breast02 trial, it significantly improved both PFS and overall survival (OS) compared to standard cytotoxic chemotherapy in the first-line treatment of metastatic TNBC patients ineligible for immunotherapy.
Professors Kim and Park concurred that ADCs are demonstrating strong efficacy in key areas of breast cancer, signaling that the time has come to shift treatment strategies.
Q. The treatment line of Enhertu has been pulled forward to first-line treatment based on the DESTINY-Breast09 study. What is the clinical significance of this study?
Professor Park: Approximately 25% of HER2-positive metastatic breast cancer patients develop brain metastases, and THP has limitations in preventing or treating this. PIK3CA mutations also predict shorter PFS. Furthermore, biomarker-related clinical studies show that patients with resistance genes like PIK3CA mutations exhibit slightly shorter PFS compared to those without such mutations.
In this context, Enhertu, which achieved significant benefits as a second-line treatment for HER2-positive metastatic breast cancer, has now been moved forward to first-line therapy. In the DESTINY-Breast09 trial, Enhertu demonstrated an unprecedented PFS of 40.7 months when used as first-line treatment. Furthermore, the study included approximately 10% of patients with pre-existing brain metastases and patients with PIK3CA mutations. Enhertu consistently demonstrated superior efficacy compared to existing first-line treatments across all patient subgroups. It is anticipated to provide clear therapeutic benefits in patient populations with significant unmet medical needs.
Q. If Enhertu is introduced as first-line therapy in practice, how should its treatment strategy be established?

Professor Kim: We should use the therapy proven to be most effective. THP remains effective, and Enhertu carries an ILD risk in approximately 10% of patients. THP (which includes the cytotoxic agent taxane) is typically given for 6–8 cycles to maximize tumor reduction, but maintaining only trastuzumab and pertuzumab therapy after 6 cycles of THP therapy can extend survival by more than 12 months.
Nevertheless, the fact that Enhertu has clearly surpassed THP therapy carries great significance. Furthermore, since HER2-positive breast cancer is inherently an aggressive type, Enhertu is likely to be the preferred initial therapy. Establishing subsequent maintenance treatment strategies is a separate issue.
Professor Park: THP can offer an excellent quality of life in select patients. Although not approved in Korea, for HER2-positive, hormone receptor-positive cases, hormone therapy can be added while maintaining Herceptin and Perjeta. Furthermore, the recently published PATINA study confirmed that adding a CDK4/6 inhibitor significantly prolongs PFS, generating considerable expectation.
While Enhertu has good therapeutic efficacy, there are some concerns regarding quality of life as well. Even if Enhertu is introduced as a first-line treatment with reimbursement in actual clinical practice, not every patient will need it in the first line. Ultimately, a strategic, individualized approach is essential.
Q. Which patients should receive the Enhertu+Perjeta combination therapy first?
Professor Park: Patients with CNS metastases from the outset or those with PIK3CA mutations are known to have slower responses or develop resistance more quickly. Patients like this, who have extensive metastases at diagnosis and a high tumor burden, need rapid tumor reduction. In these cases, the Enhertu+pertuzumab combination therapy can achieve faster tumor reduction compared to the existing THP regimen, and I believe it can be a more preferred therapy for this patient group.
Professor Kim: In the pivotal CLEOPATRA trial for the THP regimen, less than 10% of participants had previously received trastuzumab as adjuvant therapy. If Herceptin was used as prior adjuvant therapy, but recurrence still occurred, the disease could be considered more aggressive. The DESTINY-Breast09 study included such patients and still achieved a PFS of 40.7 months, making the combo’s significance even greater.
Q. How will the first-line standards change if the Enhertu combination therapy gains approval and reimbursement in Korea? Also, what is the likelihood of its reimbursement?
Professor Park: If Enhertu is approved as first-line therapy, the decision will ultimately depend on the patient's situation. In Korea, if Enhertu becomes reimbursed in the first line, patients might feel they'd be at a disadvantage if they don’t use it, leading many to want it. However, using THP therapy first doesn't eliminate the opportunity to use Enhertu later. Therefore, a thorough discussion with the patient and their family is necessary to determine which treatment to use first, considering factors like underlying diseases or quality of life.
Personally, I would likely use THP therapy first in HER2-positive, hormone receptor-positive patients, except in special cases like brain metastases, PIK3CA mutations, or high tumor burden. This is because if THP therapy is effective, adding the PATINA regimen (Ibrance(palbociclib) maintenance therapy) can sustain efficacy for a considerably long period. However, if the patient is HER2-positive or has a high tumor burden requiring rapid symptom relief, I would likely use Enhertu first.
Professor Kim: The recent DESTINY-Breast11 study compared neoadjuvant Enhertu (4 cycles) followed by THP (4 cycles) vs. cytotoxic chemotherapy (4 cycles) followed by THP (4 cycles). The Enhertu group showed a higher rate of pathological complete response (PCR), particularly in the hormone receptor-negative breast cancer subgroup, where PCR was reported at 83.1%.
Also, the DESTINY-Breast05 study reported favorable outcomes when Enhertu was administered for an additional 14 cycles to patients who did not achieve PCR after neoadjuvant therapy. In such cases, if both approaches demonstrate efficacy, a dilemma may arise regarding the optimal treatment sequence. The principle is to make decisions considering the patient's overall situation. Generally, the more effective treatment will eventually be moved to an earlier stage.
Q. I'd like to follow up on the Dartroway question. It's said that about 70% of TNBC patients cannot use immune-oncology drugs. Why do so many patients not respond to these drugs? I'm curious if the same goes for other cancer types, or if this is a characteristic unique to triple-negative breast cancer.

Professor Park: The situation has completely changed with the advent of ADC (Antibody-Drug Conjugate) drugs, which deliver the drug much more precisely. The drug being carried by the ADC was also a new agent not previously used in breast cancer treatment, and its mechanism kills cancer cells much more effectively than conventional chemotherapy drugs. Therefore, the synergy between immuno-oncology drugs and ADCs has improved the efficacy of breast cancer treatment.
Particularly for PD-L1-negative patients, only cytotoxic anticancer drugs were available until now, but even these couldn't be used long-term due to toxicity, and PFS was only around 4-5 months at best. Furthermore, many patients passed away after just 2-3 treatments, resulting in an OS of just over a year. However, with the advent of the innovative ADC anticancer drug, a clear survival extension effect has now been confirmed. Datroway, in particular, demonstrated this effect for the first time in the TROPION-Breast02 study.
Professor Kim: mmunotherapy efficacy depends on PD-L1 expression, which is present in only 30–40% of TNBC. The remaining 60-70% of patients without PD-L1 expression have no choice but to use conventional cytotoxic anticancer drugs.
Fundamentally, ADCs appear effective because they selectively target cancer cells. Previously, 60-70% of TNBC patients who were PD-L1 negative and thus unable to use immune-oncology drugs posed a problem. Recently developed ADC anticancer drugs target TROP2, which is expressed in most cancers and is relatively more prevalent in triple-negative breast cancer, making it a promising target. The emergence of these ADC anticancer drugs has created treatment opportunities for patients who previously could not use immune checkpoint inhibitors.
Q. I understand that recent discussions are leaning toward using Enhertu if there is even minimal HER2 expression. I'm curious how this discussion might change if Datroway becomes available.
Professor Park: Enhertu has not been studied as a first-line treatment in TNBC patients. If a patient has already used one other anticancer drug and shows even minimal HER2 expression, Enhertu can be considered based on findings from the DESTINY-Breast04 study. Currently, for first-line treatment of TNBC, TROP2 ADC is the only option with clinical trial data-based evidence, so the introduction of Datroway will be a new treatment option that has been previously unavailable.
Professor Kim: Based on the DESTINY-Breast04 study, if the disease progresses after using cytotoxic chemotherapy and there is even minimal HER2 expression, Enhertu can be used, though it is not yet reimbursed. Alternatively, it can be used after one course of cytotoxic chemotherapy following hormone therapy. For hormone receptor-positive breast cancer, using Enhertu before cytotoxic chemotherapy, after hormone therapy, is supported by the DESTINY-Breast06 study.
Q. For PD-L1-negative patients, two ADC options appear available. In a situation where one drug has OS data, and the other only has PFS2 data, should the drug with OS benefit be considered more valuable?
Professor Kim: A similar example is Kisqali (ribociclib) versus Verzenio (abemaciclib) in the adjuvant setting. Kisqali started development earlier and could demonstrate OS data, while Verzenio, developed later, faced difficulties in providing OS data. Therefore, ribociclib, which showed benefits in both PFS and OS, was considered the gold standard. Given the same cost, it was reasonable to choose the treatment with confirmed OS evidence.
Some argue that simply preventing cancer recurrence is meaningful enough, so meeting the primary endpoint has significance. Later, Kisqali and Verzenio were indeed found to have similar OS levels. However, since OS is the most critical indicator, under identical conditions, this patient would prefer a treatment with a confirmed improvement. Additionally, confirming treatment benefit through OS can also help secure reimbursement.
Professor Park: In Korea, reimbursement status primarily influences treatment selection.
Q. If Datroway is introduced in Korea, what role do you think it will play in TNBC treatment?
Professor Kim: Datroway can be used for patients who relapse within 6 months after treatment or within 12 months of disease-free survival. For TNBC patients, it's necessary to first confirm whether recurrence occurred within one year. Dartroway's advantage lies in its slightly different criteria in terms of recurrence compared to existing treatments.
Professor Park: The situation Professor Kim mentioned represents the patient group most urgently in need of ADCs. However, the currently available ADC anticancer drug for triple-negative breast cancer in Korea, sacituzumab govitecan, cannot be used in that specific situation. Therefore, the current approach involves first administering other treatments whose efficacy is uncertain, followed by sacituzumab govitecan as a second-line therapy. Once Datroway is introduced in Korea, it may be able to fill this treatment gap.
-

- 0
댓글 운영방식은
댓글은 실명게재와 익명게재 방식이 있으며, 실명은 이름과 아이디가 노출됩니다. 익명은 필명으로 등록 가능하며, 대댓글은 익명으로 등록 가능합니다.
댓글 노출방식은
댓글 명예자문위원(팜-코니언-필기모양 아이콘)으로 위촉된 데일리팜 회원의 댓글은 ‘게시판형 보기’와 ’펼쳐보기형’ 리스트에서 항상 최상단에 노출됩니다. 새로운 댓글을 올리는 일반회원은 ‘게시판형’과 ‘펼쳐보기형’ 모두 팜코니언 회원이 쓴 댓글의 하단에 실시간 노출됩니다.
댓글의 삭제 기준은
다음의 경우 사전 통보없이 삭제하고 아이디 이용정지 또는 영구 가입제한이 될 수도 있습니다.
-
저작권·인격권 등 타인의 권리를 침해하는 경우
상용 프로그램의 등록과 게재, 배포를 안내하는 게시물
타인 또는 제3자의 저작권 및 기타 권리를 침해한 내용을 담은 게시물
-
근거 없는 비방·명예를 훼손하는 게시물
특정 이용자 및 개인에 대한 인신 공격적인 내용의 글 및 직접적인 욕설이 사용된 경우
특정 지역 및 종교간의 감정대립을 조장하는 내용
사실 확인이 안된 소문을 유포 시키는 경우
욕설과 비어, 속어를 담은 내용
정당법 및 공직선거법, 관계 법령에 저촉되는 경우(선관위 요청 시 즉시 삭제)
특정 지역이나 단체를 비하하는 경우
특정인의 명예를 훼손하여 해당인이 삭제를 요청하는 경우
특정인의 개인정보(주민등록번호, 전화, 상세주소 등)를 무단으로 게시하는 경우
타인의 ID 혹은 닉네임을 도용하는 경우
-
게시판 특성상 제한되는 내용
서비스 주제와 맞지 않는 내용의 글을 게재한 경우
동일 내용의 연속 게재 및 여러 기사에 중복 게재한 경우
부분적으로 변경하여 반복 게재하는 경우도 포함
제목과 관련 없는 내용의 게시물, 제목과 본문이 무관한 경우
돈벌기 및 직·간접 상업적 목적의 내용이 포함된 게시물
게시물 읽기 유도 등을 위해 내용과 무관한 제목을 사용한 경우
-
수사기관 등의 공식적인 요청이 있는 경우
-
기타사항
각 서비스의 필요성에 따라 미리 공지한 경우
기타 법률에 저촉되는 정보 게재를 목적으로 할 경우
기타 원만한 운영을 위해 운영자가 필요하다고 판단되는 내용
-
사실 관계 확인 후 삭제
저작권자로부터 허락받지 않은 내용을 무단 게재, 복제, 배포하는 경우
타인의 초상권을 침해하거나 개인정보를 유출하는 경우
당사에 제공한 이용자의 정보가 허위인 경우 (타인의 ID, 비밀번호 도용 등)
※이상의 내용중 일부 사항에 적용될 경우 이용약관 및 관련 법률에 의해 제재를 받으실 수도 있으며, 민·형사상 처벌을 받을 수도 있습니다.
※위에 명시되지 않은 내용이더라도 불법적인 내용으로 판단되거나 데일리팜 서비스에 바람직하지 않다고 판단되는 경우는 선 조치 이후 본 관리 기준을 수정 공시하겠습니다.
※기타 문의 사항은 데일리팜 운영자에게 연락주십시오. 메일 주소는 dailypharm@dailypharm.com입니다.