- LOGIN
- MemberShip
- 2025-12-17 06:00:59
- ‘Imfinzi demonstrates rationale for perioperative immunotherapy in gastric cancer’
- by Son, Hyung Min | translator | 2025-12-15 11:02:47
The role of adjuvant systemic therapy is emerging as an important consideration even in patients with resectable gastric and gastroesophageal junction (GEJ) adenocarcinoma.
Despite outstanding surgical outcomes in East Asia, a significant proportion of patients with stage II-III locally advanced disease still experience recurrence due to micrometastases. In this context, a perioperative treatment strategy, which involves systemic therapy before and after surgery, has emerged as a promising approach to enhance long-term outcomes.
At the recent ESMO Asia Congress 2025 held in Singapore, results from an Asian subgroup analysis of the Phase III MATTERHORN study were presented, reinforcing the clinical value of Imfinzi (durvalumab) in combination with standard FLOT chemotherapy (5-FU, leucovorin, oxaliplatin, and docetaxel).
In the study, Imfinzi plus FLOT demonstrated clinically meaningful improvements in event-free survival (EFS), 3-year overall survival (OS), and pathological complete response (pCR). These findings signal a clear shift toward earlier use of immunotherapy in resectable gastric cancer.
Surgery remains the cornerstone of the cure in gastric cancer. However, there is growing global consensus, including in Asia, that surgery alone is insufficient for many patients. The MATTERHORN study demonstrated that administering a combination of chemotherapy and immunotherapy prior to surgery, followed by curative resection and additional therapy afterward, can significantly improve long-term outcomes.
Based on these results, the U.S. Food and Drug Administration (FDA) approved Imfinzi for the treatment of adult patients with resectable, early-stage, and locally advanced (stages II, III, and IVA) gastric and gastroesophageal junction (GEJ) cancers last month. The approved regimen includes neoadjuvant Imfinzi in combination with chemotherapy before surgery, followed by adjuvant Imfinzi in combination with chemotherapy, then Imfinzi monotherapy.
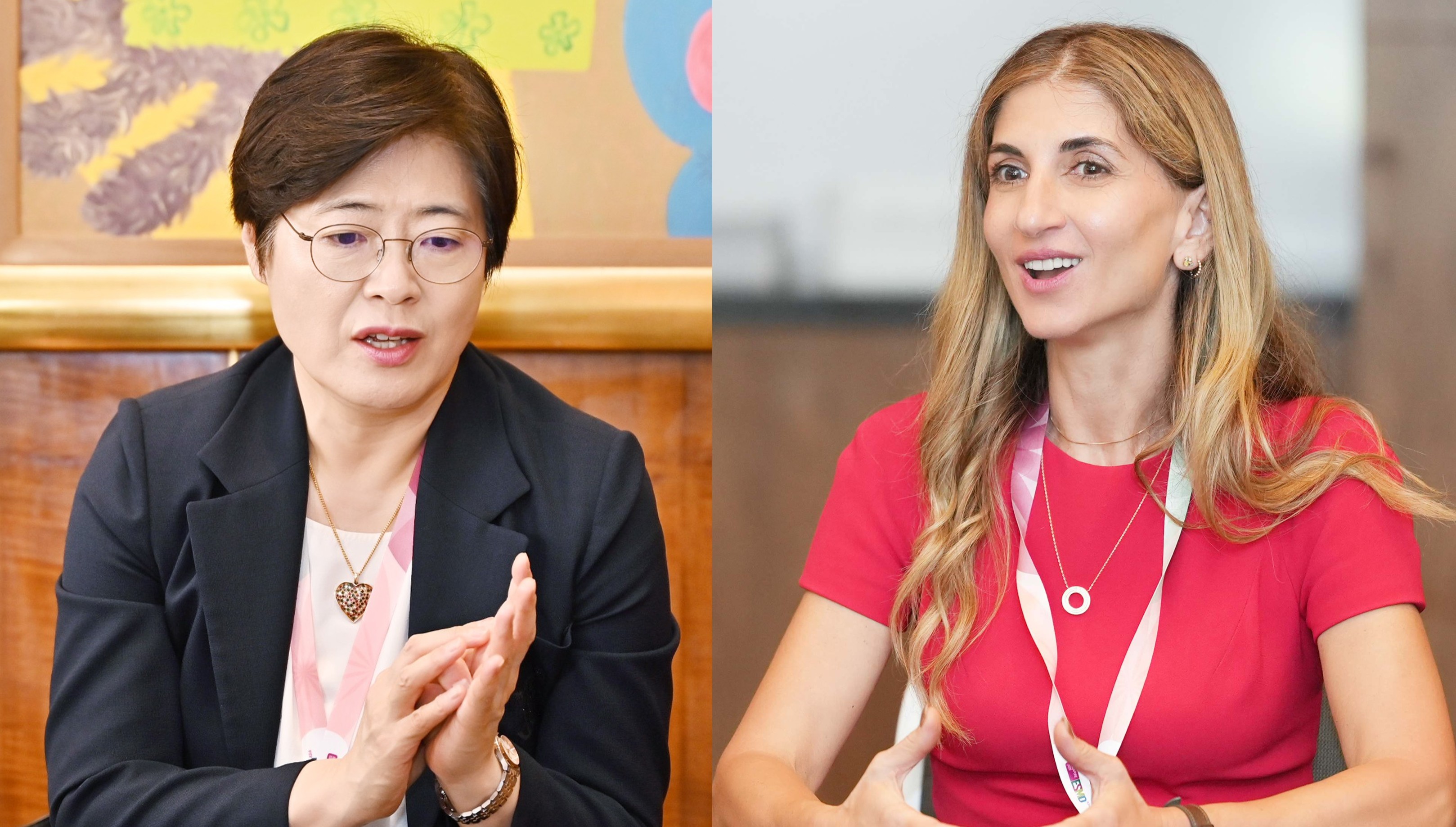
At ESMO Asia 2025, Daily Pharm spoke with Dr. Yelena Y. Janjigian, first author of the MATTERHORN study (Chief of the Gastrointestinal Oncology Service at Memorial Sloan Kettering Cancer Center), as well as Professor Sun Young Rha of Yonsei Cancer Center (President of the Korean Cancer Association) to discuss the clinical implications of this shift and the challenges associated with its implementation in Korea.
Q. As the first author of MATTERHORN, what prompted the development of this perioperative immunotherapy strategy for patients with resectable gastric and GEJ adenocarcinoma, and what is the clinical significance of the results?

Dr. Yelena Janjigian: MATTERHORN holds significance as the first Phase III study in the resectable, early-stage setting to demonstrate improvements across pCR, EFS, and OS with chemo-immunotherapy.
At ESMO Asia, we presented subgroup results from Japan, Korea, and Taiwan, which were consistent with the global findings. These data support the global relevance of the perioperative approach.
With recent FDA approval for resectable gastric and GEJ adenocarcinoma, aligning treatment approaches across regions will help us move the field forward, especially given the global incidence of more than 1.2 million new cases each year.
Q. The Asian subgroup showed efficacy and safety trends consistent with global results.
Professor Yelena Janjigian: Three key points are important. First is the feasibility across regions. Perioperative Imfinzi was deliverable in Asian centers, and physicians were able to administer both FLOT and durvalumab safely.
It also did not compromise surgical care. Rates of complete (R0) resection and the ability to proceed to surgery were maintained.
Furthermore, the results showed improvement across all major efficacy endpoints—pCR, EFS, and OS. The ability to improve all three endpoints in one study is unprecedented in this setting and underscores the strength and value of the data.
Q. What considerations should clinicians keep in mind when applying the regimen in earlier-stage patients?
Professor Yelena Janjigian: The study enrolled a broad age range—from 18 to 84 years—and older patients benefited similarly to younger patients.
That said, some patients, particularly in Asian populations, may present with nutritional compromise or lower baseline white blood cell counts. Asian investigators are familiar with these characteristics. Strategies such as early G-CSF administration and careful initial dose tailoring of FLOT can help maintain safety while preserving efficacy.
Most importantly, close clinical monitoring, hydration, and supportive care are essential components of successful perioperative treatment.
Q. Some Korean clinicians believe the regimen may be more suitable for stage III or IV than stage II. What is your view on this?
Professor Yelena Janjigian: Clinical staging in gastric cancer is often imprecise. A patient staged clinically as T2 may be found at surgery to have T3N1 disease. Because many patients have difficulty tolerating intensive postoperative therapy after major gastrectomy, preoperative treatment becomes particularly valuable.
We believe the greatest benefit of chemo-immunotherapy occurs when the tumor remains in place, allowing optimal priming and expansion of anti-tumor T-cells. This is supported by the stronger efficacy observed in the neoadjuvant component compared with adjuvant-only settings.
In my clinical practice, even patients with clinically estimated T2 tumors—especially those with diffuse or signet-ring histology—are discussed in a multidisciplinary context for consideration of perioperative systemic therapy.
Additionally, the shift in tumor epidemiology in Asia—with increasing proximal and GEJ tumors—further supports the need for downstaging approaches, as these tumors historically have poorer surgical outcomes.
Q. How should we interpret the potential for non-operative management in early gastric cancer?
Professor Yelena Janjigian: This area is highly exploratory and remains limited to very select patients within clinical trials or specialized centers.
In certain patients who achieve a complete clinical and pathologic response and who can reliably adhere to intensive surveillance, non-operative strategies have been examined. However, this is not standard practice and remains controversial, particularly among surgeons.
Nevertheless, these discussions reflect a broader evolution toward balancing cure with long-term quality of life. Gastrectomy, even when minimally invasive, alters eating patterns, sleep patterns, and body image. For selected patients, preserving the stomach—when supported by rigorous evidence and strict monitoring—could represent a meaningful advance, but this requires further research before it can be broadly implemented.
Q. Gastric cancer has historically been viewed as a disease with favorable surgical outcomes, leading to a lesser emphasis on chemotherapy. Yet MATTERHORN highlights the importance of perioperative treatment. Why is this approach necessary?

Professor Sun Young Rha: MATTERHORN enrolled patients with stage II and III gastric cancer eligible for curative surgery. While stage I “early gastric cancer” is often cured through endoscopic treatment or gastrectomy, stage II–III cancers are locally advanced and carry significantly higher recurrence risk.
In East Asia, surgery followed by adjuvant chemotherapy has historically yielded strong outcomes, with five-year survival rates around 75–80%. Still, approximately 30–40% of stage III patients experience disease relapse, demonstrating a significant unmet need.
Perioperative therapy aims to eradicate micrometastases after surgery and sustain systemic control afterward. In Western countries, perioperative FLOT has become the standard to achieve a better tumor resection, considering factors such as the increased obese population and different tumor extent at GEJ.
Q. What are the key findings of MATTERHORN, and which patients are most likely to benefit from D-FLOT?
Professor Sun Young Rha: The MATTERHORN study is significant in that it introduces a new treatment option for patients with locally advanced, resectable gastric cancer. Notably, a distinct survival benefit was observed in high-risk stage III patients with a high tumor burden. It is also noteworthy that the overall survival curve suggests the possibility that more than half of patients may remain alive at five years.
However, it should be noted that MATTERHORN did not compare the experimental arm with the post-operative adjuvant chemotherapy that has been long used in Korea or Japan, but rather with FLOT, which is considered the global standard of care. While FLOT is highly effective, Asian patients may encounter challenges in completing treatment due to its relatively high intensity.
Therefore, especially in Asia where surgical outcomes are generally more favorable, it may be more appropriate to selectively apply this regimen to patients with high-stage disease.
Q. If the D-FLOT regimen becomes available in Korea, which patients would be the most appropriate candidates?
Professor Sun Young Rha: If ongoing follow-up continues to support the favorable outcomes observed in stage III patients—particularly in terms of EFS and 3-year OS—this group will likely be prioritized in Korea.
For stage II patients, surgery followed by adjuvant chemotherapy already yields a 5-year OS rate up to 80%, and the potential incremental benefit of perioperative D-FLOT must be balanced against its higher treatment burden and toxicity profile.
In MATTERHORN, approximately 40–50% of patients completed the full perioperative regimen, reflecting the challenges associated with the adjuvant FLOT component. This underscores the importance of careful patient selection. Stage III patients, who have higher rates of micrometastatic disease and a 30–40% recurrence risk within two years, are expected to derive the greatest benefit.
Clinical features such as extensive nodal involvement, T4 tumors, or biologically aggressive histology should guide decision-making. Biomarker-informed approaches will increasingly help tailor treatment intensity and minimize unnecessary toxicity.
Q4. What distinguishes Asian patients from Western patients in MATTERHORN?
Professor Sun Young Rha: A notable feature of Asian patients enrolled in the MATTERHORN study is that they generally had good performance status and a relatively lower tumor burden. In countries such as Korea and Japan, where early detection rates are high and surgical outcomes are excellent, patients enrolled in clinical trials can potentially have better overall performance status compared to their Western counterparts.
While the proportion of stage IV patients in the study appears somewhat high, it should be interpreted as including patients with high-risk, advanced gastric cancer characterized by deep tumor invasion or extensive lymph node involvement, rather than those with unresectable or incurable M1 metastatic disease.
In the MATTERHORN study, Asian patients represented approximately 20% of the total population, indicating that additional real-world experience will be needed to further strengthen the evidence base. It will be important to continue accumulating data from Asian patients to more clearly define the clinical significance in future practice.
Q. What challenges must Korea overcome to adopt perioperative durvalumab?
Professor Sun Young Rha: Above all, aligning treatment approaches between surgeons and medical oncologists is essential. Especially in Korea and Japan, where surgical outcomes are outstanding, and the paradigm remains surgery-centric. Consensus-driven discussions with surgeons are needed to establish the role of perioperative immunotherapy in high-risk advanced gastric cancer. To ensure patients do not lose access to optimal treatment options, multidisciplinary collaboration is vital for designing comprehensive treatment plans.
From a medical oncology standpoint, individualized dose adjustment and proactive management of adverse events are key, particularly given the complexity and toxicity of the FLOT regimen. Active supportive care (such as antiemetics, G-CSF support, and dose modification) is necessary to help Asian patients complete therapy.
Finally, reimbursement is a major hurdle. Without sustainable reimbursement pathways, early real-world adoption will be limited. Generating clinical experience and real-world data, especially in high-risk stage III patients who are most likely to benefit, is important to help establish the evidence base needed for broader access.
-

- 0
댓글 운영방식은
댓글은 실명게재와 익명게재 방식이 있으며, 실명은 이름과 아이디가 노출됩니다. 익명은 필명으로 등록 가능하며, 대댓글은 익명으로 등록 가능합니다.
댓글 노출방식은
댓글 명예자문위원(팜-코니언-필기모양 아이콘)으로 위촉된 데일리팜 회원의 댓글은 ‘게시판형 보기’와 ’펼쳐보기형’ 리스트에서 항상 최상단에 노출됩니다. 새로운 댓글을 올리는 일반회원은 ‘게시판형’과 ‘펼쳐보기형’ 모두 팜코니언 회원이 쓴 댓글의 하단에 실시간 노출됩니다.
댓글의 삭제 기준은
다음의 경우 사전 통보없이 삭제하고 아이디 이용정지 또는 영구 가입제한이 될 수도 있습니다.
-
저작권·인격권 등 타인의 권리를 침해하는 경우
상용 프로그램의 등록과 게재, 배포를 안내하는 게시물
타인 또는 제3자의 저작권 및 기타 권리를 침해한 내용을 담은 게시물
-
근거 없는 비방·명예를 훼손하는 게시물
특정 이용자 및 개인에 대한 인신 공격적인 내용의 글 및 직접적인 욕설이 사용된 경우
특정 지역 및 종교간의 감정대립을 조장하는 내용
사실 확인이 안된 소문을 유포 시키는 경우
욕설과 비어, 속어를 담은 내용
정당법 및 공직선거법, 관계 법령에 저촉되는 경우(선관위 요청 시 즉시 삭제)
특정 지역이나 단체를 비하하는 경우
특정인의 명예를 훼손하여 해당인이 삭제를 요청하는 경우
특정인의 개인정보(주민등록번호, 전화, 상세주소 등)를 무단으로 게시하는 경우
타인의 ID 혹은 닉네임을 도용하는 경우
-
게시판 특성상 제한되는 내용
서비스 주제와 맞지 않는 내용의 글을 게재한 경우
동일 내용의 연속 게재 및 여러 기사에 중복 게재한 경우
부분적으로 변경하여 반복 게재하는 경우도 포함
제목과 관련 없는 내용의 게시물, 제목과 본문이 무관한 경우
돈벌기 및 직·간접 상업적 목적의 내용이 포함된 게시물
게시물 읽기 유도 등을 위해 내용과 무관한 제목을 사용한 경우
-
수사기관 등의 공식적인 요청이 있는 경우
-
기타사항
각 서비스의 필요성에 따라 미리 공지한 경우
기타 법률에 저촉되는 정보 게재를 목적으로 할 경우
기타 원만한 운영을 위해 운영자가 필요하다고 판단되는 내용
-
사실 관계 확인 후 삭제
저작권자로부터 허락받지 않은 내용을 무단 게재, 복제, 배포하는 경우
타인의 초상권을 침해하거나 개인정보를 유출하는 경우
당사에 제공한 이용자의 정보가 허위인 경우 (타인의 ID, 비밀번호 도용 등)
※이상의 내용중 일부 사항에 적용될 경우 이용약관 및 관련 법률에 의해 제재를 받으실 수도 있으며, 민·형사상 처벌을 받을 수도 있습니다.
※위에 명시되지 않은 내용이더라도 불법적인 내용으로 판단되거나 데일리팜 서비스에 바람직하지 않다고 판단되는 경우는 선 조치 이후 본 관리 기준을 수정 공시하겠습니다.
※기타 문의 사항은 데일리팜 운영자에게 연락주십시오. 메일 주소는 dailypharm@dailypharm.com입니다.