- LOGIN
- MemberShip
- 2025-12-22 00:29:57
- Company
- BESREMi lands in Big 5 Hospitals in Korea
- by Eo, Yun-Ho Mar 17, 2025 05:59am
- BESREMi, a new drug for polycythemia vera, has been approved for prescription at tertiary hospitals in Korea. According to the industry sources, PharmaEssentia Korea's BESREMi (ropeginterferon alfa-2b, a treatment for polycythemia vera, has recently passed the Drug Committees (DCs) of the Big 5 medical institutions in Korea, including Samsung Medical Center, Seoul National University Hospital, Seoul St. Mary's Hospital, Asan Medical Center, and Severance Hospital. As the drug’s reimbursement review is underway, the drug’s reimbursement listing is expected to quickly lead to actual prescriptions. Polycythemia vera is a rare blood disorder where a somatic cell mutation in the bone marrow abnormally activates bone marrow function and produces excessive red blood cells. It has a short survival period and is so fatal that 10~15% of patients with polycythemia vera develop myelofibrosis or leukemia within 10 years. Although hydroxyurea had been used as the standard of care, it was difficult to fundamentally cure the disease with hydroxyurea, and patients who could not be treated with hydroxyurea had limitations as there were practically no drugs available for them in Korea’s domestic reimbursement environment. BESREMi, an interferon treatment that selectively removes JAK2 mutations that cause polycythemia vera. In Korea, the drug received approval in October 2020 to treat low-risk and high-risk patients with polycythemia vera without symptomatic splenomegaly. The drug demonstrated its potential as a radical treatment for polycythemia vera in patients who had not received cytoreduction therapy or received less than 3 years of treatment with hydroxyurea. Therefore, whether the only interferon treatment option approved for polycythemia vera will be born in Korea is receiving attention. BESREMi demonstrated its efficacy and safety in the Phase III PROUD/CONTINUATION-PV trial that was conducted on polycythemia vera patients. Trial results showed that 53% of the patients in the Besremi arm achieved a complete hematological response, an improvement compared with the hydroxyurea patient arm (38%). The hematologic and molecular response rates at 72 months were also high, at 80.4% and 65.3% in low-risk and high-risk patients, respectively. Regardless of their risk, patients treated with Besremi did not require phlebotomy even 6 years after administration. Besremi is recommended as a first-line or second-line treatment for polycythemia vera in the National Comprehensive Cancer Network (NCCN) and European Leukemia Network (ELN) guidelines, regardless of previous treatment experience.
- Company
- Radioligand 'Pluvicto' available at tertiary gen hospitals
- by Eo, Yun-Ho Mar 17, 2025 05:59am
- Product photo of Pluvicto 'Pluvicto,' a new drug for prostate cancer, is now available for prescription at tertiary general hospitals. According to industry sources, Novartis Korea's targeted radioligand therapy, Pluvicto (Lutetium vipivotide tetraxetan), has passed the drug committees (DC) of the 'Big 5' hospitals, including Samsung Medical Center, Asan Medical Center in Seoul, Seoul St. Mary's Hospital, and Sinchon Severance Hospital, as well as the 17 medical institutes nationwide. A radioligand combines a therapeutic radioactive isotope with a ligand (targeted substance). A therapeutic radioactive isotope is released when radioligand binds to a targeted cell. This mechanism suppresses the proliferation of cancer cells. The MFDS designated Pluvicto, a treatment for metastatic castration-resistant prostate cancer (mCRPC), as the 6th medicine to be added to the 'Global Innovative products on Fast Track (GIFT)' following acknowledgment of the drug's innovativeness in June 2023. It was officially approved in May of last year. However, Pluvicto is still a non-reimbursed drug. Novartis is now preparing to apply for an insurance reimbursement listing. Pluvicto is a radioligand used to treat patients with prostate-specific membrane antigen (PSMA)-positive mCRPC who have been treated with androgen receptor (AR) pathway inhibition and 'taxane'-based chemotherapy. Pluvicto has been regarded as the next-generation innovative therapy that delivers a therapeutic radioisotope to prostate cancer cells by binding the radioisotope 177Lu to PSMA, ultimately killing cancer cells. Pluvicto was designated as an innovative drug and priority review drug by the U.S. Food and Drug Administration (FDA) and obtained FDA approval (March 2022). It was acknowledged for its innovativeness overseas. Meanwhile, the efficacy of Pluvicto was demonstrated through the Phase 3 VISION study. The combination therapy containing Pluvicto and the optimal standard therapy in study participants who have been previously treated with androgen receptor (AR) pathway inhibition and 'taxane'-based chemotherapy reduced mortality risk by 38% compared to the standard therapy alone. It has also statistically reduced the radiographic disease progression or death by 60%. Furthermore, approximately 1/3 (30%) of patients in the combination therapy group, treated with Pluvicto+standard therapy, who can be evaluated showed an objective response, compared to 2% of the monotherapy group.
- Company
- Lotte Biologics signs MOU with Asimov for CDMO business
- by Whang, byung-woo Mar 14, 2025 05:57am
- (Fromt the left) James Park, CEO of Lotte Biologics, Alec Nielsen, co-founder and CEO of Asimov Lotte Biologics (CEO: James Park) announced on the 13th that it has signed a memorandum of understanding (MOU) with Asimov, based in Boston, Massachusetts, for collaboration in the contract development and manufacturing organization (CDMO) business. Through the agreement, Lotte Biologics will provide services covering the entire process from cell line development to GMP (Good Manufacturing Practice) production by utilizing Asimov's next-generation cell line development platform technology. This is expected to further the companies’ CDMO capabilities and track record. Earlier, Lotte Biologics successfully confirmed its scale-up and mass production capabilities through a test applying Asimov's proprietary cell line development platform, CHO Edge system, at the Syracuse Biocampus. This agreement is part of a collaboration to provide full-scale end-to-end services to clients based on these achievements. Asimov's CHO Edge system is a synthetic biology-based cell line development platform that accelerates the production of antibody and protein therapeutics through the genetic design and optimization of Chinese hamster ovary (CHO) cells. In particular, it supports the rapid development of customized high-productivity and uniform cell lines by applying automated work processes and AI-based analysis. In addition, the CHO Edge system combined with Lotte Biologics' GMP manufacturing capabilities enables a smooth transition from cell line development to commercial production. The company believes that this will be an important turning point in expanding the scope of Asimov's business along with the expansion of its CDMO business. In addition, the signing of the MOU is expected to maximize the benefits of Lotte Biologics' US production base. James Park, CEO of Lotte Biologics, said, “I hope this agreement will serve as an opportunity to maximize the strengths of both companies. We will continue to provide differentiated services to our customers by bringing synergy with Asimov's technology and Lotte Biologics' production capacity, while striving to become a company that contributes to the development of the bio-industry and, ultimately, to the improvement of the quality of life of patients.”
- Company
- "More BTK inhibitor options for MCL, Brukinsa as alt choice"
- by Whang, byung-woo Mar 14, 2025 05:57am
- Changes to the treatment settings have been brought to Mantle cell lymphoma (MCL) with the launching of new treatments like BTK inhibitors and implementing reimbursement. As the 2nd-generation BTK inhibitors are introduced, treatment options have been broadened for relapsed or refractory MCL, where treatment options have been limited to 1st-generation BTK inhibitors. Dr. Youngwoo Jeon, a Professor in the Department of Hematology at Yeouido St MaryDuring a meeting with Daily Pharm, Dr. Youngwoo Jeon, a Professor in the Department of Hematology at Yeouido St Mary's Hospital, who runs the only Lymphoma and Cell Therapy-Research Center in South Korea, emphasized the need to discuss ways to effectively utilize treatment options. Mantle cell lymphoma (MCL) is a subtype of non-Hodgkin lymphoma (NHL), accounting for approximately 5% of all NHL cases. MCL shows aggressive clinical features. Unlike typical lymphoma that starts in lymph nodes, MCL occurs in organs where lymph nodes are not located. Patients often transfer from dermatology, oncology, and gastroenterology to hematology. Five years ago in South Korea, the annual new patient number was about 80. Now, that there are about 100-110 new patients each year. "According to international classification standards, extranodal T-cell lymphoma is typically considered indolent; however, once it surpasses a critical threshold, it can proliferate rapidly, like DLBCL, and requires immediate treatment," Dr. Jeon said. "Even if the disease initially progresses slowly, the short time between diagnosis and treatment means clinicians on the front lines inevitably perceive it as aggressive." In the case of MCL, the development of new treatment options, including standard therapies, has been slow, and treatment protocols or strategies have only been established relatively recently. As a result, treatment approaches have been sporadic and often based on available economic discretion, implying that patients have been treated drugs designed for other types of lymphoma treatments. Previously, combination treatments such as CHOP (rituximab+cyclophosphamide/doxorubicin/vincristine/prednisone) were primarily used. Patients with poor ECOG were administered treatments that have lower-toxicity, such as follicular lymphoma treatments like R-CVP (rituximab+cyclophosphamide/vincristine/prednisone). In addition to these options, patients have the choice to pay for BR treatment (bendamustine+rituximab) out-of-pocket. "Expanded option to include BTK inhibitors is regarded favorable, 2nd generation with reduced side-effects gains attention" The remaining issue lies in the relapse and treatment resistance seen in MCL. Many patients present with a poor prognosis at diagnosis, and given the nature of indolent lymphomas, which are notoriously difficult to cure, the sequencing of treatments becomes increasingly critical. Dr. Jeon explained, "Full recovery is challenging for indolent lymphomas like MCL. Thus, we adopt a strategy similar to that used in treating chronic lymphocytic leukemia, focusing on maximizing progression-free survival (PFS). Moreover, because relapse is frequent, it is difficult to aim for a cure from the very first treatment line, so we carefully plan the treatment sequence for when the disease relapses." In response to these unmet therapeutic needs, BTK inhibitors have emerged. In addition to the 1st-generation agents, a 2nd-generation treatment, like Brukinsa (zanubrutinib), has been introduced. Since June 2024, reimbursement for Brukinsa has been expanded to include its use as monotherapy for patients with MCL who have received at least one prior treatment. Dr. Jeon analyzed, "The introduction of oral targeted anticancer agents, such as first- and second-generation BTK inhibitors, has greatly improved patient treatment convenience. Under conventional cytotoxic chemotherapy, patients typically endured cycles of deterioration and improvement over more than a year of hospital admissions, often leading to death. Because patients can self-administer the medication and only need to manage side effects, treatment accessibility has been significantly enhanced." In fact, the 1st-generation BTK inhibitor, Ibrutinib, has shown outcomes that surpass those observed in clinical trials, as evidenced by over seven years of real-world data (RWD). "In about two years, we expect RWD on the second-generation BTK inhibitor, Brukinsa, will become available," Dr. Jeon said. "Based on results with 1st-generation BTK inhibitors, Brukinsa's data are expected to be very favorable. Although it has only been a short time, its satisfactory performance in the clinical setting is very encouraging." Dr. Jeon has highlighted that a characteristic of 2nd-generation BTK inhibitors is their enhanced selectivity for BTK. Typically, when a drug affects unintended targets, it can lead to adverse events such as cardiac hemorrhage, referred to as an off-target effect. 2nd-generation agents like Brukinsa have been designed to minimize these off-target effects. Dr. Jeon said, "These agents have reduced the incidence of hematologic bleeding and cardiac issues seen in clinical trials to around 7–8%, less than half of previous rates, which is very encouraging," adding, "However, in real-world clinical practice, we focus more on managing gastrointestinal disturbances and onycholysis, side effects that can significantly impact patient adherence during long-term treatment." "The criteria for BTK inhibitors are limiting…patient's life-long use of treatments must be considered" Despite both 1st- and 2nd-generation BTK inhibitors being eligible for reimbursement, a significant limitation remains: if a patient fails on a 1st-generation BTK inhibitor, subsequent BTK inhibitor therapy is not reimbursable. Patients only have one opportunity for BTK inhibitor treatment when considering treatment sequencing. Dr. Jeon had about five to six patients on 1st-generation BTK inhibitors that have been switched with Brukinsa. Dr. Jeon explains that while patients already stabilized on 1st-generation therapy typically continue, new patients are generally started on Brukinsa whenever possible. Yet, Dr. Jeon stressed that even though switching between 1st- and 2nd-generation therapies that both target the same molecule can be justifiable, it is critical to remember that these drugs are intended for lifelong use. "Patients on 1st-generation BTK inhibitors often suffer from severe nausea and vomiting that disrupt their daily lives. In such cases, switching to Brukinsa, which has reduced off-target effects, has produced notably positive outcomes," Dr. Jeon said. "It appears that the Health Insurance Review and Assessment Service (HIRA) considers switching unnecessary because the treatment offers a refined version of the same target," Dr. Jeon said. "Because forcing patients to endure painful side effects for a lifetime is like torture, 2nd-generation BTK inhibitors will represent an excellent alternative." Finally, Dr. Jeon emphasized the urgent need to adopt CAR‑T therapies as a third-line treatment for MCL quickly. "While CAR‑T therapy is already being implemented as third-line treatment overseas, it is not yet approved domestically, so they are available for use. However, the HIRA must propose an alternative so Korean patients could eventually receive treatment on par with those in other G20 countries," Dr. Jeon said. "Approximately 85% of patients are filtered out during second-line BTK inhibitor treatment, leaving very few who progress to third-line treatments," Dr. Jeon said. "Although these treatments are high-cost, the financial burden is likely minimal due to the small patient population."
- Company
- Takadea's metastatic colorectal cancer drug Fruzqla wins nod
- by Whang, byung-woo Mar 14, 2025 05:57am
- Takeda Pharmaceutical Korea announced on March 13 that its metastatic colorectal cancer treatment, Fruzqla (fruquintinib), received domestic marketing approval from the Ministry of Food and Drug Safety (MFDS) on March 6. The efficacy·effectiveness of Fruzqla has been demonstrated for adult patients with metastatic colorectal cancer who have previously been treated with a chemotherapy containing fluoropyrimidines, oxaliplatin, and irinotecan plus an anti-VEGF or anti-EGFR agent (for patients with wild-type RAS), and whose disease has progressed or who does not show tolerability following treatment with trifluridine/tipiracil and/or regorafenib. With this approval, a new treatment option is now available to improve overall survival for metastatic colorectal cancer patients who, due to limited options in treating later stages of cancer, have not received adequate treatment. Fruzqla is a small-molecule VEGFR-TKI that selectively targets vascular endothelial growth factor receptors (VEGFR)-1, 2, and 3, thereby selectively inhibiting the neoangiogenesis and lymphangiogenesis of cancer cells. By avoiding unnecessary targets other than VEGFR-1, 2, and 3, the drug achieves high exposure and sustained target inhibition, while its once-daily oral administration enhances patient convenience. The approval of Fruzqla was based on a Phase 3 clinical trial involving 691 adult patients with metastatic colorectal cancer who have received prior treatments. Study results showed that the median overall survival (mOS) in the Fruzqla group was 7.4 months, which is significantly longer than the 4.8 months observed in the placebo group, resulting in a 34% reduction in the risk of death. Additionally, the Fruzqla group had a median progression-free survival (mPFS) of 3.7 months, more than double the 1.8 months in the placebo group, corresponding to a 68% reduction in disease progression or death risk. Mahender Nayak, Takeda Pharmaceutical Korea' Senior Vice President for Growth & Emerging Market, stated, "Fruzqla is a new treatment option for metastatic colorectal cancer that has emerged after over a decade and can be used regardless of specific biomarkers. We expect it to offer favorable tolerability and to improve both quality of life and survival outcomes for patients who needed additional treatment options in the later stages of anticancer therapy." Nayak added, "Fruzqla is already approved in several countries worldwide, including South Korea, the United States, Europe, and Japan. Takeda Pharmaceuticals Korea will continue to work to supply innovative new drugs and enhance treatment accessibility to meet the unmet needs of cancer patients."
- Company
- GSK Korea releases myelofibrosis drug Ojjara in Korea
- by Whang, byung-woo Mar 14, 2025 05:57am
- GSK Korea announced on the 12th that it has launched Ojjara (momelotinib), a treatment for myelofibrosis, in Korea. Ojjara was approved by the Ministry of Food and Drug Safety in September last year as a treatment for adults with anemia at intermediate or high risk of myelofibrosis (primary myelofibrosis, post-polycythemia vera myelofibrosis, or post-essential thrombocythemia myelofibrosis). Ojjara has a unique triple-inhibition mechanism that blocks JAK1, JAK2, and ACVR1 (Activin A Receptor Type 1). In the treatment of myelofibrosis, inhibition of JAK1 and JAK2 can contribute to the improvement of systemic symptoms and reduction of splenomegaly in patients, while inhibition of ACVR1 can help alleviate anemia by inducing a reduction in hepcidin expression. With this launch, Ojjara is expected to significantly improve anemia, which has remained an unmet need in the domestic treatment environment for myelofibrosis, while also settling as a treatment option that can improve systemic symptoms and splenomegaly, which are existing treatment goals. Managing anemia is one of the unmet needs in the treatment of existing patients with myelofibrosis. Anemia, which increases the need for blood transfusions, causes more than just dizziness, and depending on the severity, it can lead to a serious condition that can be life-threatening. The Phase 3 SIMPLIFY-1 and MOMENTUM studies have shown that, regardless of prior treatment with JAK inhibitors, Ojjara can significantly improve the main symptoms of splenomegaly and transfusion dependence in the treatment of patients with myelofibrosis with anemia. In the SIMPLIFY-1 study, which confirmed the clinical efficacy and safety of Ojjara compared to that of JAK inhibitors in the first-line treatment of patients with myelofibrosis who had no prior experience with JAK inhibitors, Ojjara demonstrated non-inferiority to JAK inhibitors in the primary endpoint of spleen volume response at week 24 of treatment. The proportion of transfusion independence in each patient group was 66.5% for the Ojjara arm and 49.3% for the ruxolitinib arm, indicating that Ojjara showed significantly less transfusion dependency. “While JAK inhibitors, which were used in the treatment of myelofibrosis, showed effects in alleviating splenomegaly and systemic symptoms, they worsened anemia or increased the need for blood transfusions, which left an unmet need,” said Seo-yeon Ahn, Professor of Hematology & Oncology at Chonnam National University Hwasun Hospital, “Ojjara has confirmed its significant clinical value in managing anemia, which is closely related to the prognosis of patients with myelofibrosis, and we expect that its launch in Korea will contribute to improving the treatment outcomes and quality of life of more patients.” Ojjara was designated an orphan drug in Korea after demonstrating improved efficacy and safety compared to existing alternative drugs, and the fact that there are less than 20,000 people with myelofibrosis in Korea.
- Company
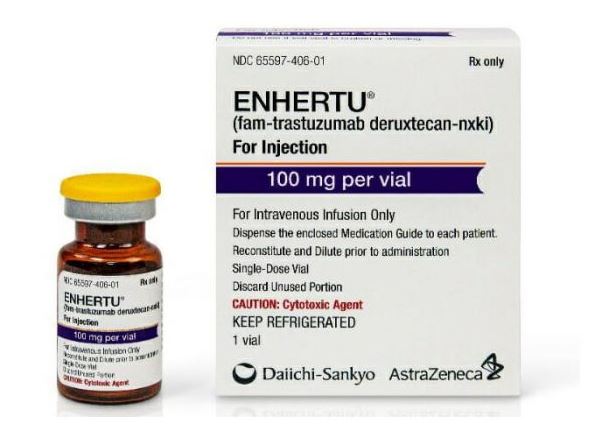
- Enhertu seeks reimb for HER2-low breast cancer and NSCLC
- by Eo, Yun-Ho Mar 14, 2025 05:56am
- The ADC anticancer drug 'Enhertu' has started a new reimbursement journey in Korea. According to industry sources, Daiichi Sankyo Korea submitted an application to receive reimbursement for two additional indications of its antibody-drug conjugate (ADC) Enhertu (trastuzumab deruxtecan) in December last year and recently began discussions with the Health Insurance Review and Assessment Service. Specifically, the company applied for reimbursement of the following indications: ▲ the treatment of patients with unresectable or metastatic HER2-low expression (IHC 1+ or IHC 2+/ISH-) breast cancer who have previously received systemic therapy in the metastatic setting or have relapsed during, or within six months of completing adjuvant chemotherapy, in the case of hormone receptor-positive (HR+) breast cancer patients, those who have received additional endocrine therapy or are not suitable for endocrine therapy; and ▲ patients with unresectable or metastatic non-small cell lung cancer with an activating HER2 (ERBB2) mutation in the tumor who have previously received systemic therapy including platinum-based chemotherapy. These indications were approved in Korea in May 2024. Enhertu was first listed as a treatment for HER2-positive breast cancer in April of the same year, but there have been persistent calls for the prompt expansion of its coverage to the HER2 low-expression indication, which is currently under discussion. In fact, a petition calling for the expansion of Enhertu’s reimbursement has garnered the support of more than 50,000 people. Therefore, it will be interesting to see whether Enhertu will be reimbursed for breast cancer patients with low HER2 expression and the newly added lung cancer indication. Meanwhile, Enhertu has confirmed its efficacy for 2 additional indications through the DESTINY-Breast04 and DESTINY-Lung02 studies. DESTINY-Breast04 compared the efficacy and safety of Enhertu and a chemotherapy regimen of the physician’s choice (capecitabine, eribulin, gemcitabine, paclitaxel, and nab-paclitaxel) in 557 patients with unresectable or metastatic HER2-low breast cancer who had previously received first or second lines of chemotherapy. Results showed that the median progression-free survival (mPFS) of the Enhertu group in the cohort of patients with hormone receptor-positive tumors was 10.1 months, demonstrating a significant improvement compared to the 5.4 months of the control group. Enhertu also reduced the risk of disease progression or death by 50% compared to the control group in the overall patient cohort, which included both hormone receptor-positive and negative tumors. In addition, Enhertu showed antitumor activity in the second-line treatment of HER2-mutated metastatic non-small cell lung cancer in the DESTINY-Lung02 study. The study evaluated the efficacy and safety of Enhertu in patients with unresectable or metastatic non-small cell lung cancer whose disease progressed after one or more systemic therapy treatments, including platinum-based chemotherapy. Results showed Enhertu recorded a confirmed objective response rate (Confirmed ORR) of 49%, complete response (CR) of 1%, and partial response (PR) of 48%, as assessed by a blinded independent central review (BICR).
- Company
- Wegovy dominates the obesity drug market
- by Chon, Seung-Hyun Mar 13, 2025 05:59am
- The introduction of Novo Nordisk's Wegovy has shaken the market substantially. Since its launch in Q4, Wegovy has captured 60% of the entire market. Given the introduction of Wegovy, the obesity market expanded to the largest in history. It also consumed the market for Saxenda, containing the same class of active ingredients as Weogvy. It is unclear whether such growth will continue because of restricted non-face-to-face medical prescriptions of obesity drugs. However, the market continues to shake up whenever effective and safe new obesity drugs from multinational companies are launched. Record sales in 2024 obesity drug market…Wegovy's Q4 sales amounted to KRW 60.3 billion, with 64% market share According to pharmaceutical market research firm IQVIA, on March 10, last year's obesity drug market amounted to KRW 236.3 billion, up 32.8% compared to the previous year. The obesity drug market continued to set the largest size for seven consecutive years since 2018, exceeding KRW 200 billion for the first time in history. Last year's growth of the obesity drug market was led by Novo Nordisk's Wegovy. Wegovy launched in October last year and recorded KRW 60.3 billion in three months. Quarterly sales figures for key products in the obesity drug market. (Legend from left) Wegovy, Qsymia, Saxenda, obesity drug market (unit: KRW 100 million, source: IQVIA) Wegovy received approval from the Ministry of Food and Drug Safety (MFDS) in April 2023. It is a GLP-1-containing semaglutide that has been shown to reduce glycated hemoglobin. While conducting clinical trials for GLP-1 diabetes treatment candidates, Novo Nordisk confirmed the effects of lowering patient body weight and developed semaglutide-containing Wegovy as an obesity drug with a once-weekly formulation. Last year's Q4 obesity market size amounted to KRW 93.8 billion, an expansion of 154.5% Year-over-Year (YoY). Wegovy accounted for 64.4% of the entire obesity drug market. Wegovy is trending globally with its outstanding weight loss effects. Wegovy recorded last year's sales of NOK 58.2 billion (About KRW 11.7 trillion), an increase of 85.7% compared to 2023 sales of NOK 31.3 billion. Since its launch in the United States, the drug has been sold out with a rapid increase in demand. Before its official launch, Wegovy was already regarded as a secret weight loss solution among celebrities, including Tesla CEO Elon Musk, and there was a global shortage. Despite being priced KRW 500,000 higher than the other drugs, Wegovy generated significant interest following its domestic launch and was in short supply. Due to the introduction of Wegovy, the sales of Saxenda and Qsymia, which previously dominated the obesity drug market, have significantly decreased. Last year, Saxenda recorded sales of KRW 65.6 billion, down 1.7% from the previous year. The decrease in sales of Saxenda was seen three years after 2021. Saxenda reported a significant decline in sales in Q4 of last year. Saxenda's sales in Q4 of last year amounted to KRW 7.3 billion, down 27.3% YoY. The sales declined by 78.9% in a quarter from KRW 18.9 billion in Q3 of last year. Analysis suggests Wegovy, a GLP-1 drug similar to Saxenda, has captured the market for Saxenda. However, Qsymia's sales have not changed much since the launch of Wegovy. Qsymia recorded sales of KRW 39.1 billion last year, up 10.1% from the previous year. In Q4 last year, when Wegovy launched, Qsymia recorded sales of KRW 9.3 billion, down 7.1% from the previous year. However, it is unclear whether Wegovy will show marked growth this year. Previously, Wegovy was prescribed through non-face-to-face medical sessions. As concerns have been raised regarding unrestricted prescription of Wegovy through non-face-to-face medical sessions regardless of weight or obesity status, the health authority discontinued non-face-to-face prescription of obesity drugs as of December 16, 2024. The obestiy drug market fluctuates whenever new drugs launch…Saxenda has led the market for the past five years The obesity drug market underwent restructuring whenever promising new products are launched. Products containing sibutramine, which inhibits appetite, sold the most and once dominated the market. However, it has no longer been in sale due to the risk of cardiovascular side effects since 2010. The Korean market of obesity drug market was sluggish for a long time. Once worth a market size of KRW 116.2 billion in 2009, it dropped to KRW 66.7 billion over five years. Since 2015, the introduction of new products has led to a rebound in the market. In February 2015, Ildong Pharmaceutical obtained domestic approval for 'Belviq,' which the company acquired from the U.S.-based Arena Pharmaceuticals and led the recovery of the entire market. Belviq selectively works on the neurotransmitter serotonin receptor, which regulates appetite and emotion, suppressing appetite and increasing meal-related satiety. It has gained attention for being the new drug approved for weight-loss medication by the U.S. Food and Drug Administration (FDA) in 13 years. Kwang-dong Pharm has contributed to the market expansion after launching 'Contrave' in 2016. Kwang-dong Pharm acquired Contrave from the U.S.-based biotech company Orexigen Therapeutics. Contrave was approved by the European Medicines Agency (EMA) in 2015, and it is used to manage the weight of adults who are overweight or obese. After the launching of Belviq and Contrave, the obesity drug market expanded to KRW 92.8 billion and KRW 96.8 billion in 2017 and 2018, respectively. Yearly obesity drug market size (unit: KRW 100 million, source: IQVIA). Belviq, Saxenda, and Wegovy were launched in 2015, 2019, and 2024, respectively. Saxenda, launched in Korea in 2018, is the first glucagon-like GLP-1 agonist medication for obesity. It contains the same ingredient as Victoza (ingredient: liraglutide), which is prescribed to patients with type 2 diabetes but with different methods of administration and dosages. Saxenda became the top-selling drug in the market after recording sales of KRW 42.6 billion in 2019, just after its launch, and maintained the place for five consecutive years until 2023. Saxenda recorded sales of KRW 66.8 billion in 2023. Saxenda took up a 37.5% market share of the obesity market in 2023. The obesity drug market set a record in 2019 with KRW 134.1 billion in 10 years. In 2023, it recorded KRW 178 billion, setting a record for five consecutive years. Qsymia, marketed by Alvogen Korea, has also contributed to the expansion of the obesity drug market. Launched in late 2019, Qsymia is a combination therapy containing 'phentermine' and 'topiramate.' Alvogen Korea secured domestic sales rights from the U.S.-based VIVUS in 2017. In late 2019, Alvogen Korea signed a co-promotion agreement with Chong Kun Dang to begin full-scale domestic sales. Qsymia recorded sales of KRW 35.5 billion in 2023. The sales of Qsymia were comparable to Saxenda. Despite oral administration, Qsymia has a relatively small amount of psychotropic drug ingredients, and it has the advantage that it can be prescribed for an extended period. Alvogen Korea's extensive sales networks in the domestic obesity market, gained from its previous experience selling Furing and Furimin, synergized with Chong Kun Dang's business power to penetrate the market with Qsymia rapidly. With the launch of Wegovy last year, the obesity drug market underwent another restructuring, and the introduction of Mounjaro and other next-generation obesity treatments is expected to reshape the landscape further. Eli Lilly’s Mounjaro received approval from the MFDS in June 2023. Mounjaro, a once-weekly injectable, is a next-generation GLP-1 analog that activates GLP-1 and GIP receptors. It has been demonstrated that Mounjaro has superior weight loss compared to Wegovy.
- Company
- "High hopes for Blincyto as consolidation therapy for ALL"
- by Whang, byung-woo Mar 13, 2025 05:58am
- Blincyto (blinatumomab), a treatment for acute lymphoblastic leukemia (ALL), is approved for an expanded indication as a consolidation therapy. Its role in clinical settings will be broadened. Experts view that having more treatment options is favorable, as the consolidation therapy option has been limited following the first-line treatment of B-precursor ALL until now. Dr. Jae-Ho Yoon, Professor in the Department of Hematology at Seoul St. MaryOn March 12, Amgen hosted a press conference celebrating the approval of an expanded indication for Blincyto as a consolidation therapy to treat B-precursor ALL. The company highlighted the potential role of the drug. On the 14th of last month, the Ministry of Food and Drug Safety (MFDS) granted approval of indication for Blincyto as a consolidation therapy for Philadelphia chromosome-negative (Ph-negative) B-precursor ALL. The approval broadened the treatment area of the drug from treating adults with relapsed or refractory B-cell precursor ALL with minimal residual disease (MRD) to treating adults of young children with Ph- B-cell precursor ALL as a consolidation therapy up to Stage 4. Patients with Ph- B-cell precursor ALL are known to relapse often despite reaching MRD negative through remission induction therapy using existing chemotherapy. Patients with ALL may experience difficulties in long-term survival despite undergoing stem cell transplantation. Therefore, ALL still has high unmet needs. Approval of a new indication for Blincyto as a consolidation therapy for patients who already had induction therapy using existing chemotherapy has gained attention since it was based on clinical data demonstrating statistically significant effects on patients diagnosed early or who relapsed. According to the E1910 clinical study results, administering Blincyto as the first-line consolidation therapy after chemotherapy to adult patients (n=112) with B-precursor cell ALL who had MRD-negative remission (
- Company
- ‘Keytruda’s 10-year milestones show its core value’
- by Whang, byung-woo Mar 13, 2025 05:58am
- Although many drugs have left their mark on the domestic pharmaceutical market, it is difficult to talk about the last decade without mentioning the immuno-oncology drug, Keytruda (pembrolizumab). As a drug that holds the title of the No. 1 in global sales, it has left various milestones in Korea, from sales to approved indications. This year marks the 10th anniversary of Keytruda’s approval in Korea, and the company is gearing up to drive another decade. The fact that Keytruda has recently been approved for a number of indications by the Cancer Disease Deliberation Committee is one of the reasons why the company's progress is drawing attention. The Oncology Business Unit of MSD Korea has been delivering its sincerity with the mindset that “cancer treatment is KEY TRUE DA (Key to the truth).” Dailypharm met with Min-kyung Kim, Associate Director (oversees lung cancer, gastrointestinal cancer, head and neck cancer, etc), and Joo-hyun Shin Associate Director (oversees breast cancer, gynecological cancer, urinary cancer, etc) of the Oncology Business Unit at MSD Korea to hear about the company’s blockbuster treatment, Keytruda. Keytruda’s 10-year approval holds title for being the immuno-oncology drug with the most indications in Korea As of February 2025, Keytruda is the most widely prescribed immuno-oncology drug in Korea indicated for 34 indications in 18 cancer types. In addition to the 2 directors who act as managers for the many indications, a total of 11 product managers (PMs) are in charge of Keytruda at MSD Korea. Specifically, under Director Kim, there are a total of 5 PMs for lung cancer, stomach cancer, biliary tract cancer, and head and neck cancer, and under Director Shin, there are a total of 6 PMs for breast cancer, gynecological cancer, and urinary cancer. Keytruda is regarded to have changed the paradigm of cancer treatment. How do the two directors feel about this? Min-Kyung Kim, Associate Director of the Oncology Business Unit at MSD Korea “Immunotherapy drugs are more effective when used early in the treatment process, when the patient's condition is good, and when used at the front line of treatment, they can bring the patients a step closer to a complete cure than before,” said Shin. “I am proud to be part of a team that is leading this change in the treatment paradigm and saving many lives.” Kim added, “I have been working at MSD for about 19 years, and I felt that all the team members are elite members who work with a great sense of mission because Keytruda is a treatment that is closely related to life. I joined the team in 2021, and I found that the team members are even more committed than they appear, and I think this is the driving force behind the growth of Keytruda over the past decade.” However, due to the vast indications for Keytruda, it is positive that there is a PM for each indication, but conversely, there may be concerns about a lack of communication or synergy between the PMs. This means that there may be concerns about the size of sales and team management. In response, the two directors emphasized that, although the role of each indication is important, a long-term strategy matters most due to the nature of Keytruda. “As the No. 1 drug, the company has organized the team with passionate and proactive PMs for the drug that collects industry-wide attention,” said Kim. “Sales are important, but we need to adjust our focus and efforts depending on new indications and momentum, and are trying to operate with clear standards while thinking about the results that can be achieved over the long term.” “The indications that are reimbursed and non-reimbursed, and the cancer types that have synergistic effects and those that do not, are creating a market or producing results,” said Shin. ”As a leader, we are constantly looking to derive new results through a process of constant feedback to see if there is anything we can do better or if there are any points to consider further.” The dilemma of expanding a treatment’s indications is 'Competition'... differentiation and market exploitation Although Keytruda has made great strides in the market over the past decade, its many indications for various types of cancers are also one of the tasks that must be resolved to compete with other treatments. Joo-hyun Shin, Associate Director of the Oncology Business Unit at MSD Korea On this, the two directors each brought up the topics of differentiation and market development, in consideration of the teams they are in charge of. So far, Keytruda has been the leading brand that has changed the paradigm of the cancer treatment environment, and has been promoting the keywords “first” and “only.” However, as these messages are gradually losing power, the company believes that it needs to promote other keywords. “Competition can also be interpreted as the threshold for immuno-oncology treatments has been lowered, which is certainly good news in this respect,” said Kim. ”However, the marketing team has a clear goal of gaining an edge over the competition, so we are focusing most on how to communicate the differentiated value of Keytruda (compared to competing products).” In addition, Shin emphasized, “From a marketing perspective, competition is not simply a matter of dividing up the market pie, but also about growing the overall size of the market, so it may be a little difficult, but we believe that it is the role of the marketing team to pioneer new markets.” There are also positive factors in the competitive situation in which Keytruda is placed. This is because it has achieved some results after applying for reimbursement for a total of 17 indications in 2023, after the 13 indications it applied for reimbursement in 2023. The Health Insurance Review and Assessment Service (HIRA) established reimbursement standards for 11 indications at the 1st Cancer Disease Review Committee (CDRC) in 2025 after 6 reimbursement attempts. The indications that passed were also diverse, including stomach cancer, esophageal cancer, endometrial cancer, rectal cancer, squamous cell carcinoma, cervical cancer, breast cancer, small intestine cancer, and biliary tract cancer. Although there are still many processes to go through, such as the Drug Reimbursement Evaluation Committee (DREC) and the National Health Insurance Service (NHIS) drug pricing negotiations, the fact that the drug passed the Cancer Disease Deliberation Committee review holds significance, as it was regarded as a reckless challenge at the time. “We took on the challenge literally recklessly with the idea that ‘Keytruda is the only option,’ to improve access to treatment for all cancer types, and I think this was possible because we all worked together with the common goal of improving patient access,” said Kim. “I feel like we're just getting started. “I think that, as Keytruda has done so far, the remaining procedures should be carried out one by one to pave the path,“ said Shin. MSD Korea’s Oncology BU Product Managers ”Keytruda’s approach to the next decade aims to expand accessibility" The two directors intuitively expressed that Keytruda is the drug that can bring about ”more tomorrows” to patients. In addition to benefiting patients, this is also the goal of the Oncology Business Unit, which is responsible for Keytruda, which is looking beyond its 10th anniversary to a new decade. In the short term, the goal is to expand the indications for which it is being reimbursed, as well as newly approved or pending indications such as endometrial cancer and stomach cancer. “The primary goal is to grow the newly approved indications and to do well until the launch of new indications because there are still indications waiting to be approved,” said Shin. ”The most important thing is to improve patient access to treatment, and we will always think about and work on how to provide good treatment options to more patients.” Next, Shin cited the birth of new drugs that will bring about another paradigm shift as the most anticipated part of the coming decade. “MSD is investing heavily in clinical trials in Korea, which is a global leader in clinical trials, with more than 5,000 people in 500 centers in Korea alone. I believe that another innovative drug will arise as a result of this investment and effort, and in that sense, I think it would be good to look forward to the company’s next 10 years.”