- LOGIN
- MemberShip
- 2025-12-22 00:29:57
- Company
- SK Chemical signs a joint sales agreement with Viatris
- by Lee, Seok-Jun Mar 06, 2025 05:58am
- SK Chemicals, which developed the first natural drug for osteoarthritis in Korea, ‘Joins Tab,’ has secured additional pain medications for its portfolio. SK Chemical (CEO Jae-Hyun Ahn) announced on the 5th that it has signed a distribution and sales agreement with Viatris Korea for △Lyrica, △ Neurontin, and △ Celebrex. Under the agreement, SK Chemicals will be responsible for the distribution of the three drugs to all hospitals and marketing to hospitals and clinics with less than 300 beds. Marketing to general hospitals with more than 300 beds will be handled by Viatris Korea. △ 'Lyrica', a treatment for peripheral and central neuropathic pain △ 'Neurontin', a treatment for neuropathic pain △ 'Celebrex', an anti-inflammatory analgesic, are products whose efficacy and safety have been confirmed through various clinical studies. SK Chemicals plans to maximize synergies with its existing products, such as ‘Joins’ and ‘Ultracet,’ by expanding its lineup of pain treatment products through this agreement. In the case of the osteoarthritis treatment drug, Joins, which is SK Chemicals' representative pain medication, and the non-narcotic anti-inflammatory analgesic drug, Ultracet, which is exclusively sold by SK Chemicals, the two are actively used in combination with the three Viatris products, so the collaboration is expected to bring synergy between the products. Hyunsun Park, Head of the Pharma Business at SK Chemicals, said, “The introduction of Lyrica, Neurontin, and Celebrex will provide patients and medical staff with a wider range of effective pain treatment options. We will continue to secure new pipelines that are highly linked to existing businesses and strengthen our expertise in specialized markets such as pain treatments.”
- Company
- Vyndamax is reimbursed for ATTR-CM in Korea
- by Whang, byung-woo Mar 06, 2025 05:58am
- Pic of Vyndamax Pfizer Korea announced on the 5th that its Vyndamax (tafamidis), a treatment for wild-type or hereditary transthyretin amyloidosis cardiomyopathy (ATTR-CM), has been granted reimbursement by Korea’s National Health Insurance. ATTR-CM is a progressive rare disease in which the naturally circulating transport protein in the blood, transthyretin (TTR), becomes unstable and separates into misfolded monomers, which accumulate in the heart and cause restrictive cardiomyopathy. According to this announcement, Vyndamax may be prescribed with reimbursement in adult patients aged 18 or older who have been diagnosed with hereditary ATTR-CM. Also, wild-type patients who satisfy all of the following conditions may receive the drug with reimbursement: those who ▲are Class I-III in the New York Heart Association (NYHA) heart failure severity classification for the last six months, ▲have received a diagnosis of heart failure and a history of one or more hospitalizations due to heart failure within the last six months, ▲has 600 pg/mL or higher level of pro-B-type natriuretic peptide (NT-proBNP, N-terminal pro-B-type natriuretic peptide level), and ▲have a left ventricular wall thickness at the end of diastole that is 12 mm or more. Vyndamax, which is the first and only approved treatment for adult patients with ATTR-CM in Korea, has secured clinical evidence through the ATTR-ACT study and the ATTR-ACT LTE study. In the ATTR-ACT study, which was conducted to compare the efficacy and safety of Vyndamax and placebo in 441 ATTR-CM patients, about 71% of patients in the tafamidis meglumine group were alive at the 30-month follow-up, showing improved survival compared to the placebo group (about 57%). It also reduced the relative risk of heart-related hospitalizations (0.48/year) by 32% compared to placebo (0.70/year) (95% confidence interval, 0.56-0.81). In addition, according to the results of the ATTR-CM LTE trial, which analyzed long-term survival rates of patients, the patient group that continued to receive tafamidis meglumine showed a reduction in all-cause mortality compared to the patient group that switched from placebo to tafamidis meglumine. Ji-Eun Lee, Head of the Specialty Care Business Unit at Pfizer Korea, said, ” We are pleased to be able to improve the access to treatment for our ATTR-CM patients who have had difficulty using the treatment due to financial constraints despite the availability of this option rather than heart and liver transplantation. We will continue to work to provide innovative treatments to patients with rare diseases, including ATTR-CM, and improve the treatment environment.”
- Company
- Novo Nordisk Korea appoints Kasper Roseeuw Poulsen as new GM
- by Whang, byung-woo Mar 06, 2025 05:58am
- Kasper Roseeuw Poulsen, Novo Nordisk Korea On March 5, Novo Nordisk Korea announced the appointment of Kasper Roseeuw Poulsen as the new General Manager starting March 2025. The new GM Kasper Roseeuw Poulsen joined Novo Nordisk in 2006 and served key roles in finance, strategy, organizational development, commercial partnership, and management across Europe, South America, and Asia-Pacific. Kasper Roseeuw Poulsen holds a bachelor's degree in Business Administration and a master's degree in Finance & International Business from Aarhus University's School of Business, Denmark. Until recently, he served as Vice President of Finance and Operations for Novo Nordisk's APAC region, overseeing more than 20 countries. Before that, he demonstrated outstanding strategy and executive ability as Vice President of a subsidiary in China. Kasper Roseeuw Poulsen said, "South Korea is a key market in the APAC region and a leading country for healthcare optimized for innovative medical settings. I'm excited to lead Novo Nordisk Korea." "By establishing closer partnerships with healthcare professionals and key healthcare partners in South Korea, we will strive to provide better benefits for patients based on Novo Nordisk's leadership in chronic diseases," he said. Meanwhile, the former GM Sasha Semienchuk was promoted to CVP Marketing in Novo Nordisk's subsidiary in China and will oversee commercial activities across the Chinese mainland. Since his appointment as Novo Nordisk Korea's GM in October 2022, Sasha Semienchuk had executed Novo Nordisk's patient-centered corporate value in the APAC region with his outstanding leadership. Sasha Semienchuk led the supply of products, such as Wegovy, for various treatment areas and fostered a corporate culture that embraces mutual growth between the company and its employees. He made significant contributions at Novo Nordisk, which earned international recognition as a 'Great Place to Work' and 'Best Workplace for Women' in two consecutive years.
- Company
- Pfizer launches JAK inhibitor for severe alopecia areata
- by Whang, byung-woo Mar 06, 2025 05:58am
- Pfizer Korea will launch a new Janus kinase (JAK) inhibitor treatment Litfulo (ritlecitinib tosilate), and set to challenge the market for severe alopecia areata. Previously launched Olumiant (baricitinib), the first drug approved in South Korea for treating adult patients with severe alopecia areata, has already settled in the market. The company will likely promote Litfulo's broader indication to treat adolescents over 12 years of age. Dr. Chong Hyun Won, Professor in the Department of Dermatology at Asan Medical Center in SeoulOn March 5, Pfizer Korea hosted a press conference celebrating the launch of the severe alopecia areata treatment Litfulo. The company highlighted the clinical significance of the drug. Litfulo is the first drug among alopecia areata treatments in South Korea to obtain approval for use in adolescent patients. Alopecia areata is an autoimmune disease that causes hair loss in the scalp, face, and body in patches or complete loss of hair. It is an inflammatory and immune-mediated disease caused by the immune system attacking the body's hair follicles, leading to hair loss. In South Korea, the number of patients treated for alopecia areata showed an increasing trend for the past 10 years, recording 154,380 patients in 2013 and 178,009 patients in 2023. In most cases, alopecia areata without severe symptoms naturally recover and respond well to treatments. However, it has a high relapse rate, with about 40-80% of patients experiencing relapse within a year. Dr. Chong Hyun Won, Professor in the Department of Dermatology at Asan Medical Center in Seoul, who attended the press conference, said, "About 100% of the patients with alopecia areata experience relapse within 20 years, so the disease has a high recurrence rate." Dr. Won explained, "It causes a substantial psychological burden on patients and is closely associated with mental health issues, such as depression, affecting the quality of life greatly." However, the introduction of JAK inhibitors like Litfulo has changed the treatment settings. Previously, severe alopecia areata was treated with corticosteroids or cyclosporine. Analysis suggests that aggressive treatment is possible after the introduction of a new option. "The launch of the new treatment provides hope for patients with unmet needs who suffered for a long time from alopecia areata. It is also meaningful to doctors, considering that a safe new option is now available," Dr. Won said. The basis of approval for Litfulo was the global clinical study Phase 2b/3 ALLEGRO. The analysis results evaluating the primary endpoint, the patient ratio with a Severity of Alopecia Tool (SALT) score of 20 or below, showed that at week 24, 23% of the patient group had a SALT score less than 20, which was statistically significant treatment effectiveness compared to a 2% in the placebo group. At week 48, the treatment group with a SALT score less than 20 was 43%, confirming significant treatment effectiveness than the placebo group (10%). This indicates that effectiveness increased over time. (from left) Dr. Chong Hyun Won, Professor in the Department of Dermatology at Asan Medical Center in Seoul, and SungBum Jung, Chief Medical Affairs at Pfizer When Olumiant was launched earlier, the alopecia areata had high unmet needs despite its non-reimbursed indication. It was evaluated that a higher-than-expected number of patients are opting for treatment. In other words, since Olumiant already dominates the market, the company must strategize to promote Litfulo. The most significant difference is the mechanism and indication. Unlike Olumiant, which targets JAK1 and 2, Litfulo primarily targets JAK3. Also, Olumiant is used for adults aged 18 and older, whereas Lifulo is used to treat adolescents aged 12 years and above. Dr. Won commented regarding this, "As of 2023, adolescents account for about 10% of the patients with alopecia areata, and the number can be lower with severity. However, the drug presents significance considering that earlier occurrence of alopecia areata may require longer treatment and has poor prognosis when relapse." Furthermore, Dr. Won mentioned that it is too early to determine drug switching between existing treatments and new treatments. "As drug switching requires the analysis of drug's effects and safety, a clear answer is not available at this point," he said. "We need confirmation of which patients can be better treated with existing treatment with longer safety."
- Company
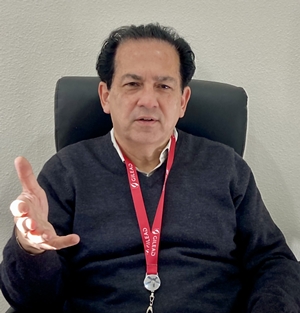
- "COVID-19 response has changed to protect high risk groups"
- by Whang, byung-woo Mar 05, 2025 06:01am
- As COVID-19 transitioned to the endemic phase, an important issue has arisen regarding 'how' to prevent and respond to the disease, unlike the initial period focused only on response. One of the big changes was the reimbursement of treatments. On October 25, 2024, The Ministry of Health and Welfare (MOHW) approved the National Health Insurance reimbursement of the COVID-19 treatments, Veklury and Paxlovid. Based on the demands of clinical settings, the government aims to provide a stable supply of COVID-19 treatments to patients through the National Health Insurance system. In another point of view regarding infectious disease management in the endemic period, experts are highlighting the need to revisit the discussion of 'SARS-CoV-2,' which is one of the respiratory viruses other than COVID-19. Essy Mozaffari, Gilead Sciences Medical AffairsDuring the meeting with Daily Pharm, Essy Mozaffari, affiliated with the Gilead Sciences Medical Affairs, emphasized the role of antiviral therapy in protecting immune-compromised individuals and high-risk patients. In February 2020, the WHO officially announced the name for COVID-19, and at the same time, it assigned the name SARS-CoV-2 to the virus. It means that corona 19 (COVID-19) is typically used when discussing symptoms, whereas the SARS-CoV-2 virus causes the infection. Medical Affairs Mozaffari (hereafter, MA) said, "At the current endemic phase, it is crucial that we discuss SARS-CoV-2 infection rather than using the term COVID-19," adding that, "If SARS-CoV-2 is used to describe the virus, it will help remind that it is a virus that can make people ill every year." The latest COVID-19 responses have focused on immune-compromised individuals and high-risk patient groups, who can be relatively vulnerable to a disease. The approach has been limiting the spread of the disease through immunization and providing treatments to infected individuals in a timely manner. For instance, the COVID-19 treatment Veklury (remdesivir) is the first antiviral agent to receive approval from the U.S. FDA for the treatment of hospitalized adult patients with COVID-19. Veklury is now recommended as the standard therapy for adults and children who are hospitalized due to SARS-CoV-2 infection. Also, it is recommended for use in non-hospitalized patients with mild and moderate symptoms who are at risk of advancing to severe COVID-19. MA Mozaffari stated, "Although there are many antiviral therapies, Veklury has low drug interaction, so it is an important treatment option for patients who must take other medicines. Patients who have liver and spleen dysfunction can use the therapy without adjusting the dosage." "Veklury with real-world evidence demonstrated effects in high-risk patient group" MA Mozaffari particularly highlighted that Veklury has proven real-world evidence (RWE) in hospitalized patients due to COVID-19. "The Phase 3 PINETREE trial involving high-risk non-hospitalized patients infected with SARS-CoV-2 has shown that administering Veklury for three days decreased the hospitalization risk," MA Mozaffari said. "The recent real-world data (RWD) confirmed that the use of Veklury in the high-risk patient group, including immune-compromised individuals and older patients aged 65 and above, significantly lowered the death risk compared to the control group in all mutation periods. MA Mozaffari views that proper management of infection through treatments can benefit the efficient management of the medical healthcare system as medical healthcare system resources are being spent on managing immune-compromised individuals. "COVID-19 infection causes a significant burden to the medical healthcare system consistently, and it poses a risk of disease progression and death in older people aged 65 and above," MA Mozaffari said. "Antiviral therapies with proven treatment effects for various COVID-19 mutations will play a crucial role in future COVID-19 treatments." Now, Gilead Sciences is conducting research on the potential use of Veklury in a particular patient group with unmet needs for COVID-19 treatments. The company is evaluating the effects of Veklury treatment in new mutations as COVID-19 vaccines target changes. "Based on trial results so far, Veklury continued to maintain treatment effects on all mutations, including omicron sub-variants. Notably, there have been no key genetic changes affecting targeted RNA polymerase of the virus," MA Mozaffari explained. The results indicate that mutations to the virus will not cause significant changes to RNA structure and function, so the therapy can continue to work effectively," MA Mozaffari analyses. Lastly, MA Mozaffari mentioned the concern for effective responses amid COVID-19 settling down as an endemic disease. "COVID-19 is now transitioned to endemic disease, but SARS-CoV-2 continues to pose significant health risk worldwide," MA Mozaffari said. "The government, researchers, doctors, and individuals must strive to maintain the infection rate low and stay alert to respond to new mutations effectively."
- Company
- Ocrevus is reimbursed for relapsing multiple sclerosis
- by Whang, byung-woo Mar 05, 2025 06:00am
- Pic of Ocrevus On March 4, Roche Korea announced that its multiple sclerosis treatment drug Ocrevus (ocrelizumab) will be reimbursed by Korea’s National Health Insurance from March 1. According to the new announcement, Ocrevus will be covered as a monotherapy for patients with relapsing multiple sclerosis, which includes ▲patients with relapsing-remitting multiple sclerosis (RRMS) who are ambulatory and have failed or had insufficient response to first-line treatment (e.g., interferon beta-1b) and ▲patients with secondary progressive multiple sclerosis (SPMS). As a result, Ocrevus will be reimbursed for the relapsing-remitting type as a second-line treatment and the secondary progressive type as a first-line treatment. Relapsing multiple sclerosis (RMS) includes both relapsing-remitting and secondary progressive multiple sclerosis. Relapsing-remitting multiple sclerosis (RRMS) is the most common type of multiple sclerosis. The reimbursement application of Ocrevus was based on a wealth of clinical evidence on its utility, including the results of large-scale global Phase III clinical trial OPERA I & II and the 10-year analysis of the open-label extension study in patients with relapsing multiple sclerosis. In the OPERA I & II studies, the Ocrevus group showed a 40% improvement in the risk of confirmed disability progression (CDP) compared to the control group over 12 weeks and maintained a consistent effect over 24 weeks. The annual recurrence rate (ARR) was reduced by nearly half compared to the control group, and the average number of brain lesions per MRI scan was also significantly improved, confirming clinical efficacy. The clinical efficacy of Ocrevus was maintained even after 10 years of dosing. A 10-year follow-up analysis conducted in the open-label extension study of OPERA I & II showed that the Ocrevus-treated group achieved a steady decline in ARR over 10 years, with the 10-year ARR (0.017) being equivalent to approximately 1 relapse in 60 years. In particular, in both clinical studies, patients who received early treatment with Ocrevus in the early stages of the clinical trial showed more effective disease progression control and lower risk of disability compared to patients who started treatment later. No new adverse reactions or unexpected side effects were observed in patients who received Ocrevus for 10 years, confirming an overall favorable safety profile. “Recently, treatment for multiple sclerosis has been shifting to a strong initial treatment strategy that actively prevents disability by using high-potency drugs from the early stages,” said Professor Ho-jin Kim of the Department of Neurology at the National Cancer Center. ”With the reimbursement of Ocrevus increasing the treatment options, more patients can effectively prevent disease progression and disability from the early stages, ultimately improving treatment outcomes.” “Ocrevus, which has risen to record number one in global drug sales at Roche, is a representative multiple sclerosis treatment that has benefited more than 350,000 patients worldwide,” said Ezat Azem, General Manager of Roche Korea. “We expect that the reimbursement application will strengthen the accessibility of treatment for patients with relapsing multiple sclerosis in Korea and provide more patients with the therapeutic benefits of Ocrevus, which have been confirmed through a large number of clinical data and prescription experiences.” Meanwhile, in Korea, Ocrevus was approved by the Ministry of Food and Drug Safety in May 2024 for two types of patients: relapsing multiple sclerosis (RMS) and primary progressive multiple sclerosis (PPMS).
- Company
- Pfizer’s sales fall 76% in 2 yrs with the end of pandemic
- by Son, Hyung Min Mar 05, 2025 06:00am
- Pfizer Korea’s sales are on a downward trend. The company's sales have plummeted by 76% in 2 years. The analysis is that the demand for COVID-19 vaccines and treatments has fallen sharply, which has affected the decline in sales. Pfizer Korea aims to make a rebound in sales with new products such as Prevnar 20, a new pneumococcal vaccine, and a COVID-19 vaccine that can respond to new variants. According to the Financial Supervisory Service on the 4th, sales of Pfizer Korea fell 51% from KRW 1.6018 trillion in 2023 to KRW 783.7 billion last year. Operating profit fell 57% from KRW 63.8 billion to KRW 27.2 billion over the same period. This is the first time in 4 years since 2020 that Pfizer Korea has recorded sales of less than KRW 1 trillion. Prizer Korea suffered a direct hit to its sales in the endemic. The company entered the KRW 1 trillion club in sales in 2021 with its COVID-19 vaccine, Comirnaty Inj, and its COVID-19 treatment, Paxlovid, but its sales have dropped sharply with the stabilization of the COVID-19 pandemic. Pfizer Korea Pfizer joined forces with BioNTech in March 2020, when COVID-19 began to spread around the world, to develop a messenger ribonucleic acid (mRNA) vaccine. BioNTech, which owned the mRNA technology, and Pfizer, which has extensive experience in large-scale global clinical trials, have produced synergy. Pfizer succeeded in developing the vaccine Comirnaty, which has a 95% preventive effect, in less than a year after the spread of COVID-19. In December 2020, the US Food and Drug Administration (FDA) granted emergency use authorization, and emergency use authorization was granted in Korea as well in March of the following year, after which the vaccine was supplied through the Korean subsidiary in earnest. Afterward, Pfizer succeeded in developing the COVID-19 treatment Paxlovid, which the Korean government also procured to use as a treatment. As a result, sales at Pfizer Korea also increased significantly. The company's sales reached KRW 1.694 trillion in 2021, surpassing the KRW 1 trillion mark, and then rose sharply to KRW 3.2254 trillion in 2022. Compared to the sales in 2020, sales increased by 723% in 2 years. However, sales began to decline in 2023 as governments around the world declared an end to the COVID-19 pandemic. Sales of Pfizer Korea in 2023 fell 50% year-on-year to KRW 1.6018 trillion, and the company failed to secure sales of KRW 1 trillion last year, at KRW 783.7 billion. Last year's sales were down 76% from 2022 when the company made the highest performance ever. Operating profit was also struggling. After recording an operating loss of KRW 7.2 billion in 2020, the company succeeded in turning a profit in 2021 with KRW 59.2 billion. After that, its sales jumped to KRW 120.1 billion in 2022 but decreased 47% to KRW 63.8 billion in 2023. Last year, it decreased by 57% from the previous year to KRW 27.2 billion. Aims to boost sales with the new product launch PfizerPfizer Korea is aiming to boost sales with the launch of a new product. The company launched a new pneumococcal vaccine, ‘Prevnar 20,’ in November last year. Prevnar 20 is a new pneumococcal vaccine that Pfizer introduced 14 years after the release of Prevnar 13. This vaccine adds seven serotypes (8, 10A, 11A, 12F, 15B, 22F, and 33F) to the 13 serotypes in the existing Prevnar 13. In clinical trials, Prevnar 20 demonstrated immunogenicity and tolerability against 20 serotypes when administered to healthy infants four times. These results were similarly shown in clinical trials conducted on adults. Sales growth is also expected for the non-small cell lung cancer drug Lorviqua. Currently, Pfizer Korea is in negotiations with the National Health Insurance Service to expand the reimbursement coverage of Lorviqua as a first-line treatment. Lorviqua is Pfizer’s third-generation ALK-positive non-small cell lung cancer targeted therapy. Currently, Takeda's Alunbrig and Roche's Alecensa, along with Lorviqua, have been fiercely competing in the second-generation ALK-positive non-small cell lung cancer targeted therapy. It will be interesting to see if the company can stay ahead of the competition in the first-line treatment environment, as the company confirmed Lorviqua’s efficacy with the latest data from the 5-year trial. Pfizer also plans to launch new vaccines that can respond to new variants to defend its sales. Pfizer introduced Comirnaty JN.1, a COVID-19 vaccine that can respond to new variants, including JN.1 last year. The company is also aiming to rebound sales by recently launching Comirnaty JN.1 0.033, a COVID-19 vaccine for infants, to make a rebound in sales.
- Company
- Reimbursement possible for Long-acting HIV treatment in KOR
- by Whang, byung-woo Mar 04, 2025 05:57am
- Expectations are growing in the clinical field with the imminent reimbursement of the long-acting HIV (human immunodeficiency virus) treatment ‘Vocabria+Rekambys’ combination in Korea. It has been more than two years since the combination was approved in Korea, but it has not yet been released on the market due to hurdles including costs. As patients have been waiting for its release, it is expected to quickly gain influence with reimbursement coverage. Pic of VocabriaAccording to industry sources, GSK Korea concluded drug price negotiations with the National Health Insurance Service for the combination therapy of the new HIV drugs Vocabria (cabotegravir) and Rekambys (rilpivirine). Rekambys Janssen Korea’s product and GSK was in charge of its reimbursement listing process in Korea. Both drugs were originally developed as oral medications and then developed into injectable drugs. Long-acting injectable drugs cannot cure HIV infection, but they are therapeutic agents that target white blood cells to help lower and maintain the level of the AIDS virus. In February 2022, it was approved by the Ministry of Food and Drug Safety as a combination therapy for the treatment of HIV-1 infection in adult patients who are virologically suppressed, have no history of virological failure, and have no known or suspected resistance to cabotegravir or rilpivirine. Currently, the market is divided between the three-drug combination therapy, Biktarvy (bictegravir/emtricitabine/tenofovir alafenamide, B/F/TAF) and the two-drug combination therapy, Dovato (dolutegravir/lamivudine). Although many prescriptions have been made before Biktarvy and Dovato, like Gemvoya and Triumeq are still being prescribed, the weight has shifted to using the later released treatments. According to the pharmaceutical research institution IQVIA, Biktarvy’s sales in 2023 had been KRW 54.5 billion, the highest among HIV treatments. This is an 11% increase compared to the KRW 49.1 billion in sales in 2022. Dovato also has a growth curve of KRW 13.2 billion in 2021, KRW 20.3 billion in 2022, and KRW 26 billion in 2023, after generating KRW 1.8 billion in sales at the time of its reimbursement approval in 2020. The biggest strength of the Vocabria+Rekambys combination that has emerged in this situation is its convenience. While existing HIV treatments are oral drugs that must be taken every day for 365 days a year, the combination therapy that includes Vocabria can reduce the frequency of administration to a maximum of six times a year with intramuscular injections administered once a month or once every two months. This strength is regarded to be effective in alleviating the anxiety of social stigma, which is considered a challenge for people living with HIV. According to a survey conducted by Love for One, an organization for people living with HIV, 73% of people living with HIV in Korea said they were afraid that taking HIV medication would reveal their infection to others and the surrounding environment. As there are already inquiries from patients about the combination therapy Vocabria+Rekambys in the clinical setting, experts believe that there will be a lot of switching of treatments. “The existing treatment requires taking one pill every day, so people have to take it in the middle of work or face stressful situations such as business trips or travel,” said Jin-nam Kim, a professor of infectious diseases at Hanyang University Hospital. ”Even before its release, there were patients who inquired about the treatment because they could avoid having to think about their daily lives if they could just get a shot at the hospital once a month.” As the number of treatments that require periodic injections, such as rheumatism and atopic dermatitis, has increased, it is believed that this may reduce the burden of social stigma felt by patients. However, the combination therapy of Vocabria+Rekambys is not all-encompassing, so the influence of existing treatments is expected to remain. Conventional treatments are usually prescribed at a hospital visit every 3 months, and in some cases, every 6 months. However, since the combination therapy is an injectable, the patient must follow the dosing cycle, and if it is difficult to shorten this cycle according to individual circumstances, it may be a burden to visit the hospital more frequently. Professor Kim said, “Adherence to medication is important, and in the case of oral medications that are taken daily, if the patient has the existing medication, they can take it daily and maintain the drug concentration. However, although there is a seven-day margin before and after the administration date for injections, there are indeed limitations depending on the patient.” The combination therapy of the two drugs is expected to be reimbursed by the National Health Insurance soon after it is approved by the Health Insurance Policy Deliberation Committee. In response, Professor Kim said that he could not make a definite statement as no treatment has been released yet, but based on patient inquiries, he expected that at least 10% of patients would switch. He added, “Injectable drugs cause pain at the injection site, and there are new drugs, so I don't think many will change at once. Still, the number of patients who inquired was in the double digits (more than 10%), and since the efficacy has already been proven through various studies, some patients will switch when provided with more options.”
- Company
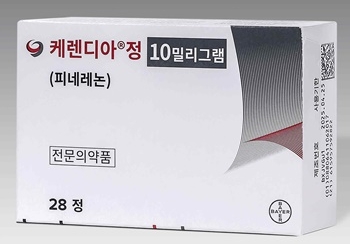
- Potential blockbuster drug Kerendia…1yr since reimbursement
- by Whang, byung-woo Mar 04, 2025 05:57am
- The prescription performance of Kerendia (finerenone), Bayer’s treatment for chronic kidney disease in adults with type 2 diabetes, has been increasing since it was granted reimbursement last year. With its monthly sales recording KRW 1 billion in the last month of last year, the drug is rapidly building up its performance, and given its growth, it is likely to become a blockbuster treatment in Korea this year. Pic of Kerendia Tab Kerendia is a first-in-class, selective, non-steroidal mineralocorticoid receptor antagonist(MRA) that inhibits the overactivation of mineralocorticoid receptors, which can cause inflammation and fibrosis in the kidneys, kidneys, and blood vessels. Kerendia, which was approved in Korea in May 2022, was approved for insurance reimbursement benefits on February 1 of last year, about a year and a half after its approval in Korea. The standards for Kerendia’s reimbursement are as follows: Adult patients with type 2 diabetes who have been taking angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) for more than four weeks, but have ▲a urinary albumin-to-creatinine ratio (uACR) over 300 mg/g or a urine dipstick test result of 1+ or higher, and ▲an estimated glomerular filtration rate (If eGFR is between 25 and 75, the drug may be administered together with ACE inhibitors and ARBs). Kerendia gained the spotlight as diabetes accounts for the highest proportion (38.6%) among the causes of end-stage renal disease. Until now, drugs to control blood pressure and reduce the burden on the kidneys were used with GLP-1 and SGLT-2 inhibitors to control blood sugar, but there was an unmet need. In particular, as there had been no drug that could directly suppress chronic inflammation or fibrosis of the kidneys, Kerendia, which has a new mechanism of action that can directly target these, is expected to play a greater role. “So far, GLP-1 receptor agonists, SGLT-2 inhibitors, and RAS inhibitors, which are blood pressure medications, have been used to treat patients with diabetes and kidney disease, but the risk of chronic kidney disease persisted in the patients,” said Yong-Ho Lee, Professor of endocrinology at Severance Hospital and Director of General Affairs of the Korean Diabetes Association. “As Kerendia has proven its efficacy in various clinical trials, it will become an important treatment option for patients with chronic kidney disease,” he said. Monthly Sales of Bayer In fact, Kerendia‘s sales have been growing since its reimbursement in Korea. After being granted reimbursement last year, Kerendia’s monthly sales started at KRW 30 million in March and continued to rise, reaching KRW 100 million in April. In particular, the company recorded monthly sales of KRW 1 billion in December, the last month of last year, and is expected to continue to increase its influence this year. Looking at the quarterly figures, the company showed twofold growth each quarter, posting KRW 800 million in the second quarter, KRW 1.7 billion in the third quarter, and KRW 2.7 billion in the fourth quarter. Taking this into account, sales are expected to easily exceed the KRW 10 billion mark which is the threshold for a blockbuster drug in Korea, within this year. The expansion of the prescription of Kerendia seems to have been influenced by its characteristics as a treatment for chronic kidney disease patients with Type 2 diabetes. According to UBIST, prescriptions increased significantly in the early days after the reimbursement was applied, mainly in the field of nephrology, but the number of prescriptions in the field of endocrinology also increased from September, and in December, when monthly sales reached KRW 1 billion, the number of prescriptions in the field of nephrology and endocrinology did not differ significantly. Quarterly Sales of Bayer In this situation, the drug’s influence in the market is expected to continue to grow as Bayer Korea announced plans to expand Kerendia’s indications. On November 20, 2019, the Ministry of Food and Drug Safety approved a randomized clinical trial to determine the efficacy and safety of finerenone on the morbidity and mortality of heart failure patients with a left ventricular ejection fraction of 40% or more who were hospitalized due to an acute non-reversible episode of heart failure. It can be regarded as a domestic version of the Phase III FINEARTS-HF trial, which evaluated Kerendia in patients with heart failure with a left ventricular ejection fraction of 40% or more, which was announced at the European Society of Cardiology's annual conference (ESC 2024) in September last year. As Kerendia has already been shown to prevent heart failure-related secondary events in patients with heart failure with reduced ejection fraction (HFmrEF) and heart failure with preserved ejection fraction (HFpEF), which have ejection fraction 40% or higher, the indication expansion in Korea is not expected to be difficult if there are no major variables.
- Company
- Commercialization of PAH drug 'Winrevair' imminent
- by Eo, Yun-Ho Mar 04, 2025 05:57am
- Product photo of Winrevair The new drug 'Winrevair' for pulmonary arterial hypertension (PAH) is anticipated to land in South Korea. According to industry sources, MSD Korea's Winrevair (sotatercept), the world's first inhibitor therapy to treat PAH, has passed the secondary evaluation for the approval-reimbursement linkage process and now enters the last phase of the review. Considering that a typical review time for drug candidates submitted to the 'Pilot Project for Integration of Product Approvals, Reimbursement Coverage Reviews, and Drug Price Negotiations' has shortened to 81.5 days, the approval for Winrevair will be made soon. Since the reimbursement review has also started, it is to be closely watched whether Winrevair will gain presence as a treatment option in South Korea. Winrevair was designated an orphan drug by the Ministry of Food and Drug Safety (MFDS) in January and designated as the Global Innovative products on Fast Track (GIFT) in April. Additionally, the U.S. Food and Drug Administration (FDA) officially approved Winrevair as a subcutaneous injection administered once every 3 weeks to treat PAH. Winrevair is designed to bind the protein complex activitin and transforming growth factor-β (TGF-β). This drug works by inbiting abnormal signaling bewteen pulmonary vascular endothelial cells and reversing the disease progression. PAH is caused by narrowing of pulmonary arteries, leading to an increase in pulmonary artery pressure, and ultimately resulting in cardiac failure. In South Korea, almost half of the patients with PAH die within 5 years. More than 10 drugs have been approved to treat PAH, including phosphodiesterase type 5 (PDE5) inhibitors and endothelin receptor antagonists. However, many patients suffer from serious symptoms despite undergoing 2-3 combination therapies. Meanwhile, the effectiveness of Winrevair compared to the placebo was confirmed in the Phase 3 study of Winrevair named STELLAR. The clinical study evaluated the effectiveness and safety of the drug, assigning patients to the Winrevair treatment group and the placebo group on 1:1 ratio. The clinical study results have shown that Winrevair extended 6 Minute Walk Distance (6MWD), the primary efficacy endpoint, by 40.1m. The placebo reduced the 6MWD by 1.4m. 38.9% of the patients treated with Winrevair had significantly improved multiple endpoints, including improvement in the secondary endpoint increase in 6MWD over 30m. This was about four-fold longer than 10% of the placebo group.